Table of contents
Written by Lynn Enright
Illustrated by Sabrina Bezerra
“Never Google Your Symptoms”, a parodic song performed by four male performers dressed in white coats, has had more than 3 million views on YouTube.
The basic gist of the ditty is this: Google is a search engine and cannot be expected to interpret your symptoms with any degree of subtlety and insight so instead of feeling reassured by your search results, you may be unnecessarily alarmed.
It’s a fairly standard viewpoint—leave your health queries to the experts, we are regularly told. The problem is that the experts don’t always have the best track record when it comes to listening to women about pain—and subsequently treating it.
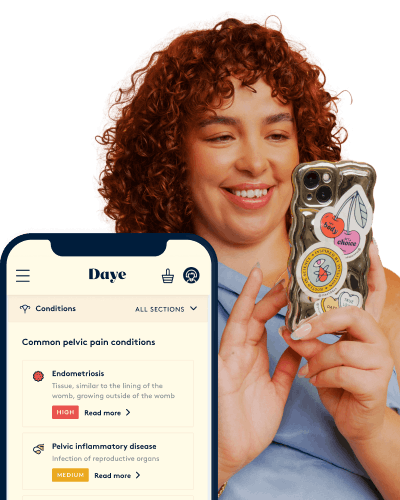
Take the pain out of your period
90% of us experience period pain, and when left unmanaged it leads to us losing 150 million productive work days per year.
Do doctors ignore women’s pain more?
In 2017, the National Institute for Health and Care Excellence (NICE) actually deemed it necessary to tell NHS doctors that they must “listen to women” who presented with symptoms of endometriosis.
It seems like weirdly obvious advice but, when you consider that it takes an average of 7.5 years to get an endometriosis diagnosis, it becomes clear that it was necessary.
Women’s pain is consistently taken less seriously than men’s—we know this anecdotally and from academic research. Women wait longer for treatment in A&E departments than men, according to studies and data from Europe and the US. And when women do see a doctor, they are more likely than men to receive prescriptions for sedatives—rather than pain medication.
Black women, women of colour and LGBTQ people, face even more barriers when seeking medical treatment, with discrimination and ignorance contributing to dangerous oversights. In 2018, Stonewall published research that showed one in seven LGBTQ people avoid accessing healthcare for fear of discrimination from staff.
In 2019, research revealed the shocking fact that Black women are 5 times more likely to die in pregnancy or from complications after childbirth than white women.
“Black people have worse health outcomes across the board,” says Miss Adeola Olaitan, a London-based consultant gynaecological oncologist, specialising in the diagnosis and treatment of all types of gynaecological cancers.
“A recent paper from America shows that they fare worse from ovarian cancer regardless of treatment modality. The reasons are complex and multifactorial and frankly, most people putting forward theories are guessing at the reasons. We need to research this clearly, suspending assumptions—and not treating Black people as homogeneous as there are as many differences within this racial group as there are between Black and white people.”
Luckily, the medical profession is changing, and there are trailblazing doctors, scientists, writers and charity organisations advocating for a system that is better and safer, but the individual must be aware that this is the landscape in which they are a patient.
Dr. Alyson McGregor is an American emergency room doctor, a professor of emergency medicine and the author of the recently published book Sex Matters: How Male-Centric Medicine Endangers Women's Health And What We Can Do About It.
“We need to wake up, individually and collectively, to the reality of being female in our current medical system,” she writes in the first chapter of her book.
“This isn’t a single-layered issue of bias or faulty protocol. Every part of our current medical system—from research and analysis to medical education, from diagnostic testing to prescribing guidelines—needs to evolve at the same time, starting now.”
I ask her why it takes so long for most women to get an endometriosis, for example. “Endometriosis is a challenging diagnosis to make,” she says. “It is not visual on exam, often is missed on ultrasounds and CT scans. The physician has to go on the patient’s insistence that there is something wrong. You can imagine how frustrating that is for women patients.”
How to advocate for yourself at the doctor
So, what can a patient who is experiencing pain and unusual symptoms do? Should she ever resort to Google, despite what the YouTube song tells us? “The best way to advocate for yourself is to stay educated—yes, this means Dr. Google—and come prepared with questions,” McGregor says.
“View your physician as an informed consultant in your healthcare. Be open about your motives for the encounter�—do you want a diagnosis? Pain relief? Questions answered? Specialist referral? This way, you will leave feeling as though you achieved your primary goal at the very least.”
If you suspect that you have a specific condition—like endometriosis or vulvodynia or ovarian cancer—you should let your doctor know. There is no point in Googling your symptoms if you’re going to keep your amateur diagnosis, and your fears, to yourself.
Miss Olaitan says clarity and preparation is key when people go to the doctor. “It is really important for the patient to be clear about her symptoms where possible: when it started, what triggers it, whether it is cyclical, i.e. related to periods, and the severity,” she says.
“If she has an idea of what she thinks may be wrong, she should tell the GP. For example, the average GP sees one case of ovarian cancer every 5 years and may not consider the diagnosis so it is perfectly reasonable for a patient to say ‘Do you think these symptoms are indicative of ovarian cancer?’ The patient should seek a second opinion if she is not satisfied that her symptoms are being addressed.”
When I talk to women (both cis and trans) and non-binary people about accessing healthcare, relating to sexual and reproductive health, it is clear that a second opinion is often necessary.
Dead ends or long delays in getting a diagnosis are depressingly frequent, especially with conditions that aren’t very common or well understood. Women live with chronic debilitating pain because their doctors don’t understand the gravity of the situation. In particularly dire instances, life-threatening diagnoses can be missed.
Louise, 23, from South Wales, lived with what she calls “quite obvious symptoms of endometriosis” for years before getting a diagnosis. Due to the severity of the pain, she was forced to take significant breaks from her education on three separate occasions. She was unable to have sex. She estimates that she visited her GP more than 50 times throughout her teens. When she was sent for an ultrasound, she was told that the cysts on her ovaries were simply a sign that she was “really young and really fertile”.
“
She was told that the cysts on her ovaries were simply a sign that she was “really young and really fertile”
At university, Louise confided in a tutor about her symptoms, and her tutor suggested that she might have endometriosis. “I properly looked into it—I used Google and the Endometriosis UK website,” she says.
“I was horrified when I did because I ticked every box and felt angry at myself for letting it get so bad.” She eventually saw a consultant, who performed a laparoscopy to diagnose and treat her condition.
Finding the time, energy—and, not least, money—to seek out second opinions and specialist care is not always straightforward. In the UK, you do not have a legal right to a second opinion within the NHS, but you can always ask your GP to arrange a second opinion, either from a specialist or another GP. Most will agree to do so and if they refuse, you do have a legal right to change your GP.
Empower yourself by keeping notes about your own health and the tests and examinations you have had. Track your menstrual cycle. Prepare for a doctor’s appointment by writing out your symptoms and your aims. Google your symptoms.
It is enraging and upsetting to know that you might encounter ignorance, discrimination or indifference when you seek treatment. It is horrifying to think that doctors may minimise your pain—but by learning how to be a better advocate for yourself and your body, you can at least help to care for yourself as the system slowly changes around you.






