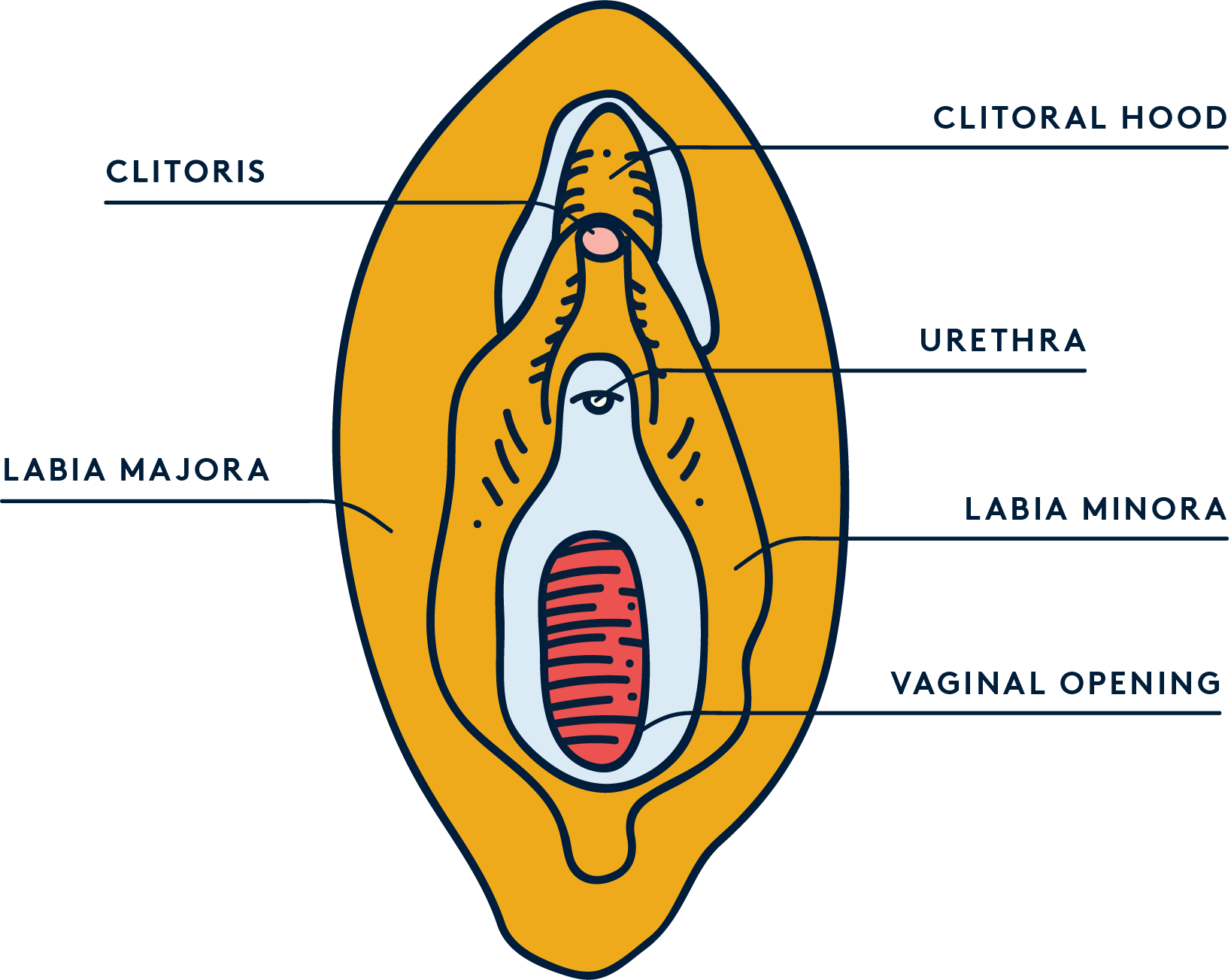
Illustrated by Sabrina Bezerra
It’s no secret that your vulva is a fairly sensitive area of your body, so it’s common to experience vulvar pain or discomfort at some point in your life.
Vulvar pain can be a temporary symptom of infection or an inflammatory condition. Sometimes, however, it can be a chronic idiopathic condition—which means it shows up spontaneously and for no known reason.
Certain infections can cause vulvar pain. If you’ve ever had the misfortune of dealing with thrush, you’ll know it can cause discomfort like swelling and itching of the vagina and vulva.
Similarly, STIs like chlamydia, gonorrhoea and trichomoniasis can sometimes cause a burning or painful sensation, but typically only when you pee or have intercourse. Lichen sclerosus and lichen planus—two skin conditions that affect the genital area—can also cause intense irritation and soreness of the vulva.
However, when vulvar pain is idiopathic it’s classified as vulvodynia.
Vulvodynia
Vulvodynia is a chronic, often disabling condition that causes pain and discomfort of the vulva and can make everyday activities like sex and using tampons incredibly painful.
As a very misunderstood condition, there are no official statistics on how many women struggle with vulvodynia. It’s believed to affect around 4-16% of women, and a US study of almost 5,000 people suggested that about 1 in 6 women have experienced the symptoms for more than 3 months during their lives.
Women with vulvodynia may also be 2 to 3 times more likely to have other chronic pain conditions, such as fibromyalgia and IBS, suggesting a link between vulvodynia and inflammatory disease.
Vulvodynia causes burning, stinging or irritation, that doesn’t have an identifiable cause and isn’t visible. It can affect the entire vulva (generalised vulvodynia) or only affect a certain part of the vulva such as the clitoris or vaginal opening (localised vulvodynia).
On top of that, both generalised and localised vulvodynia can both be provoked or unprovoked, meaning the pain can show up out of nowhere, or be brought on by certain activities.
Penetrative sex, inserting a tampon, sitting for a long period of time, or even simply wearing tight-fitting trousers can cause vulvodynia to flare up in some people.
As with many gynaecological issues, vulvodynia is severely under-researched and misunderstood, which makes diagnosing and treating the condition very difficult.
Because of its unknown cause, many doctors still believe that it’s nothing more than a psychosomatic condition associated with mental health.
Despite its high prevalence, vulvodynia is still often dismissed as a psychological condition. Unsurprising, since women are more likely to be prescribed sedatives, rather than painkillers, and our pain is more often dismissed as “perceived” (ie. it’s all in our head) compared to men.
Vulvodynia is also sometimes referred to as a “depressed vagina”, which is disconcerting for several reasons—chief among them that it affects the vulva, not the vagina…
It’s also due to the fact that since it can be a frustrating and debilitating condition, sufferers often experience symptoms of depression and anxiety, so antidepressants and cognitive behavioural therapy are commonly prescribed as a treatment for vulvodynia.
The diagnostic process can be lengthy because it involves excluding other causes of vulvar pain (such as allergies, inflammation or infections) before treating for vulvodynia.
Part of the problem with diagnosis is also that vulvodynia doesn’t have any visible symptoms, and the lack of research also means the exact cause of vulvodynia is unknown.
Although the cause is unknown, researchers have a number of theories as to what causes vulvodynia, including a sensitivity to thrush.
Even though a history of recurrent vulvovaginal candidiasis (thrush) is reported by women with vulvodynia, there isn’t enough evidence to prove specific bacterial or fungal infections are a cause of vulvodynia.
If you have vulvodynia, there are some measures you can take to ease symptoms and reduce discomfort. These include avoiding any products that are irritating, such as feminine hygiene products, douches, fragranced tampons or pads, and douching. It’s also recommended that you only wear cotton underwear, use lube during intercourse (as long as it’s not fragranced or flavoured!), and only wash your vulva with water.
TL;DR
- Several things can cause vulvar pain, including infections or inflammatory diseases. When vulvar pain is consistent and doesn't have a specific cause, it's classified as vulvodynia.
- Despite it affecting almost 16% of people with a vulva, it's a very under-researched and misunderstood condition.
- Vulvodynia causes burning, stinging or irritation of the vulva that isn't visible and often shows up unprovoked. It can affect the entire vulva (generalised vulvodynia) or only affect a certain part of the vulva (localised vulvodynia).
- Diagnosing and treating vulvodynia is a complex, lengthy process that can sometimes include antidepressants and cognitive behavioural therapy.