Written by Liv Cassano
Illustrated by Sabrina Bezerra
Endometriosis is a condition where the cells similar to the uterine lining start to grow in other places of the body, including the ovaries, fallopian tubes, and bowels. It can cause severe pain and heavy periods.
These growths (also referred to as “lesions” and “implants”) act like the endometrium, reacting to the hormonal fluctuations of the menstrual cycle and building up every month, then shedding like a period.
But unlike the endometrium, which exits through the cervix and vaginal canal, the blood has nowhere to go and remains trapped inside the body. This leads to inflammation and pain, and creates scar tissue on organs.
What is endometriosis?
Endometriosis is a chronic disorder that affects around 1 in 10 women and AFAB individuals of any age, and can cause uncomfortable symptoms like abnormally painful and heavy periods, bowel and bladder problems, and often difficulty conceiving.
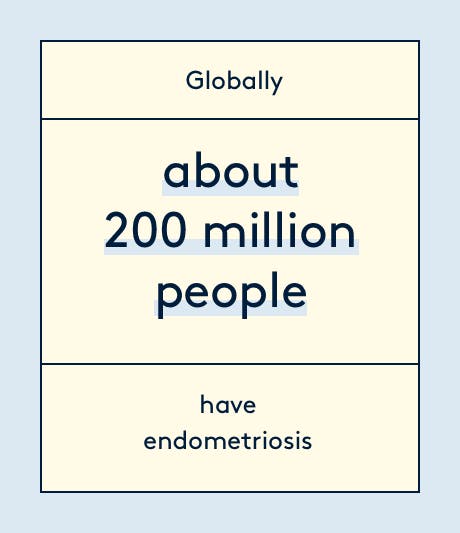
Despite it affecting 1.5 million women in the UK, and about 200 million worldwide, there’s very little awareness of what the condition entails and how to manage it.
Endometriosis is so under-researched that MPs launched an inquiry into women's experiences of endometriosis. According to the 2020 All Party Parliamentary Group (APPG) on Endometriosis inquiry, the average diagnosis time for endometriosis increased from seven and a half to eight years. So not only has diagnosis time not improved in the past decade, but it's actually getting worse.
The APPG surveyed over 10,000 people with endometriosis as well as healthcare practitioners, and found that prior to getting a diagnosis 58% visited their GP more than 10 times, 43% visited doctors in hospital over 5 times and 53% visited A&E.
Once diagnosed, only 19% know if they are seen in an endometriosis specialist centre, and 90% would have liked access to psychological support, but were not offered this.
Take the pain out of your period
90% of us experience period pain, and when left unmanaged it leads to us losing 150 million productive work days per year.
Endometriosis symptoms
Part of the mystery surrounding endometriosis is that everyone experiences the chronic condition differently. Symptoms can vary greatly from person to person, and many women may have no noticeable symptoms.
But for others, the condition can be extremely debilitating and seriously affect their quality of life. Typical symptoms of endometriosis include:
- Abnormally heavy and painful periods, which often cause women to miss school or work, and not get out of bed.
- Painful bowel movements and urination
- Chronic fatigue
- Pain during and/or after intercourse
- Pelvic and lower back pain, which typically gets worse during your period
- Nausea, constipation or diarrhoea, especially during your period
- Difficulty conceiving
Endometriosis symptoms are usually progressive, so they often start as intense period pain, and worsen over time.
Endometriosis can be a very difficult condition to live with, not only physically but also mentally. The toll endometriosis takes on your body often interferes with patients’ education, career and personal relationships, and the emotional stress can make you more likely to have anxiety, depression, or other mental health issues.
Causes of endometriosis
The cause of endometriosis is unknown, but there are several theories as to why it may happen.
It’s believed that genetic factors may play a role in endometriosis, as the condition often runs in families and affects certain ethnic groups more than others. However, there is no definite proof that endometriosis is hereditary.
Another theory is that the endometrial cells spread through the body via the lymphatic system or the bloodstream, which could explain why on rare occasions endometriosis tissues has been found outside of the pelvic and abdominal area.
The most widely accepted theory is retrograde menstruation, where rather than leaving your body like normal, the endometrium flows upwards, through the fallopian tubes, and attaches itself to other organs. However, retrograde menstruation doesn’t explain why endometriosis can occur in people who have had a hysterectomy.
None of these theories fully explain what causes endometriosis, and the condition is likely to be due to a combination of factors. Without knowing for certain what the cause is, it’s hard to diagnose and treat the condition, which is why more research on endometriosis is desperately needed.
Endometriosis diagnosis
The average diagnosis time for endometriosis in the UK is eight years, although it can sometimes take more than ten.
The symptoms of endometriosis vary significantly and can often be similar to other conditions. In fact, endometriosis is often misdiagnosed as IBS, PCOS, fibroids, or an STI.
Since endometriosis doesn’t show up on blood tests or scans, the only definitive way to diagnose endometriosis is by a laparoscopy – a surgery where a surgeon passes a thin tube through a small cut in your belly and look for any patches of endometriosis tissue. If they find any lesions, the tissue can be removed and inspected under a microscope to confirm that it is endometrial tissue.
Unfortunately, the reality of being diagnosed with endometriosis is not as straightforward. Endometriosis patients are often overlooked, and their symptoms dismissed despite their severity.
Female pain is often brushed off in the medical community (a little something called the gender pain gap), and women are more likely to have their pain discounted as emotional or psychogenic rather than real pain, and results in not being treated as well as men. A lot of the time, endometriosis is chalked up to nothing more than a “bad period”.
It’s crucial to remember that periods (whether or not you have endometriosis) don’t have to be painful – and they certainly shouldn’t interfere with your life to the point of sacrificing your career, studies or social life.
Although people with periods are often told to grin and bear it, if the pain is so severe that you can’t go about your everyday life, it’s not something you have to put up with. To make matters even more complicated, painful or heavy periods aren’t always a symptom of endometriosis.
In 2017, the National Institute for Health and Care Excellence (NICE) issued guidelines for the NHS in stating that if women have symptoms including continuing pelvic pain, severe period pain, pain during sex or they suffer from infertility, conditions like endometriosis should be investigated.
Endometriosis treatment
There is currently no cure for endometriosis, but there are treatments that can help with symptoms. Unfortunately, the delay in diagnosis means a delay in treatment initiation.
Endometriosis symptoms are usually managed with over the counter or prescription painkillers, hormone treatments – like certain contraceptive methods or medicine such as gonadotrophin-releasing hormone (GnRH) analogues) – and surgery.
The goal of hormone treatments such as the combined oral contraceptive pill (COCP) is to stop the hormonal fluctuations that cause the endometrium to build and shed every month, to reduce the amount of bleeding, inflammation and pain that happens during the menstrual cycle.
“Hormonal contraception is widely used and helpful in the management of endometriosis,” says Dr. Nicola Tempest, a research fellow at Liverpool Women’s Hospital specialising in endometriosis and fertility.
“Hormonal contraception in its different forms help to decrease the amount of bleeding a woman has, decrease pain and improve quality of life. The hormonal contraceptives help different women to different extents, for some women they are enough treatment to not require further medication or surgeries and for others this is not the case.”
None of these treatments will stop the endometriosis from recurring, but they can be effective management tools. Even in the case of surgery, treatment usually requires a multi-tiered approach that includes lifestyle changes.
“Endometriosis is an oestrogen dependent chronic inflammatory disease, which means that if oestrogen is present (when a hysterectomy is performed and the ovaries are left), then endometriosis can definitely still be present. If women want more permanent relief from endometriosis, then ovaries need to be removed,” adds Dr. Tempest.
Diet, exercise, stress management and alternative therapies may relieve symptoms, but there is little evidence to support this. “No good literature exists documenting the use of behavioural therapy, recreational drugs, reflexology, homeopathy, psychological therapy or exercise for the management of pain in endometriosis,” explains Dr. Tempest.
“The Royal College of Obstetrics and Gynaecology acknowledges that some women who seek complementary and alternative medicine may benefit from these, but they do not recommend their use as their benefits and/or harm are unclear.”
Ultimately, the effectiveness of treatment depends on how severe the condition is, and the person’s overall health. It’s important to always discuss any type of treatment with your healthcare provider first.
Endometriosis can be a very difficult condition to deal with, from diagnosis to treatment. If you think you may have endometriosis, it’s helpful to keep a detailed account of all the symptoms you’re experiencing to show your doctor – and being vocal about it.
TL;DR
- Endometriosis is a chronic condition where tissue similar to the lining of the uterus starts to grow in other places, such as the ovaries and fallopian tubes.
- Although symptoms of endometriosis can vary from person to person, it can cause intense pain and heavy periods.
- It’s unclear what causes endometriosis, which makes diagnosing the condition even harder. The average diagnosis time in the UK is eight years.
- There is currently no cure for endometriosis, and treatment includes lifestyle changes, hormonal medication, or surgery.
For more advice and support, visit Endometriosis UK and Know Your Endo.