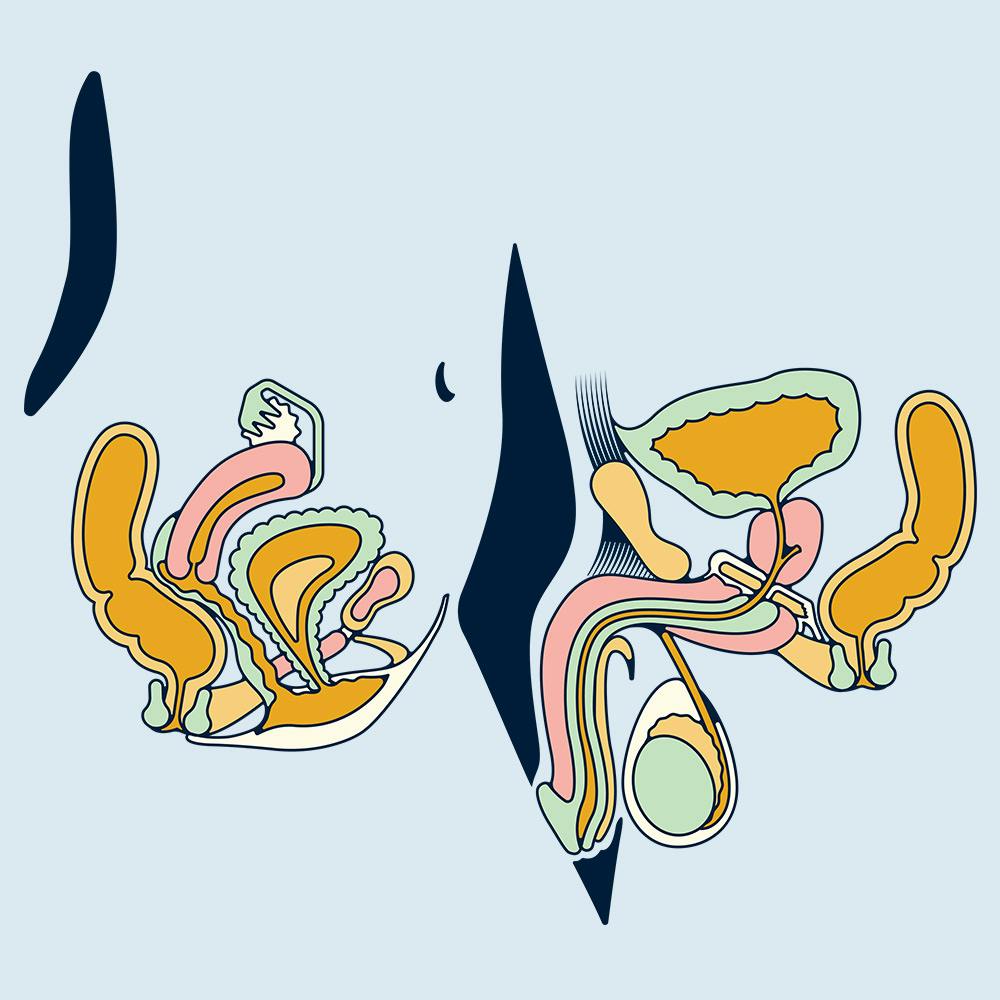
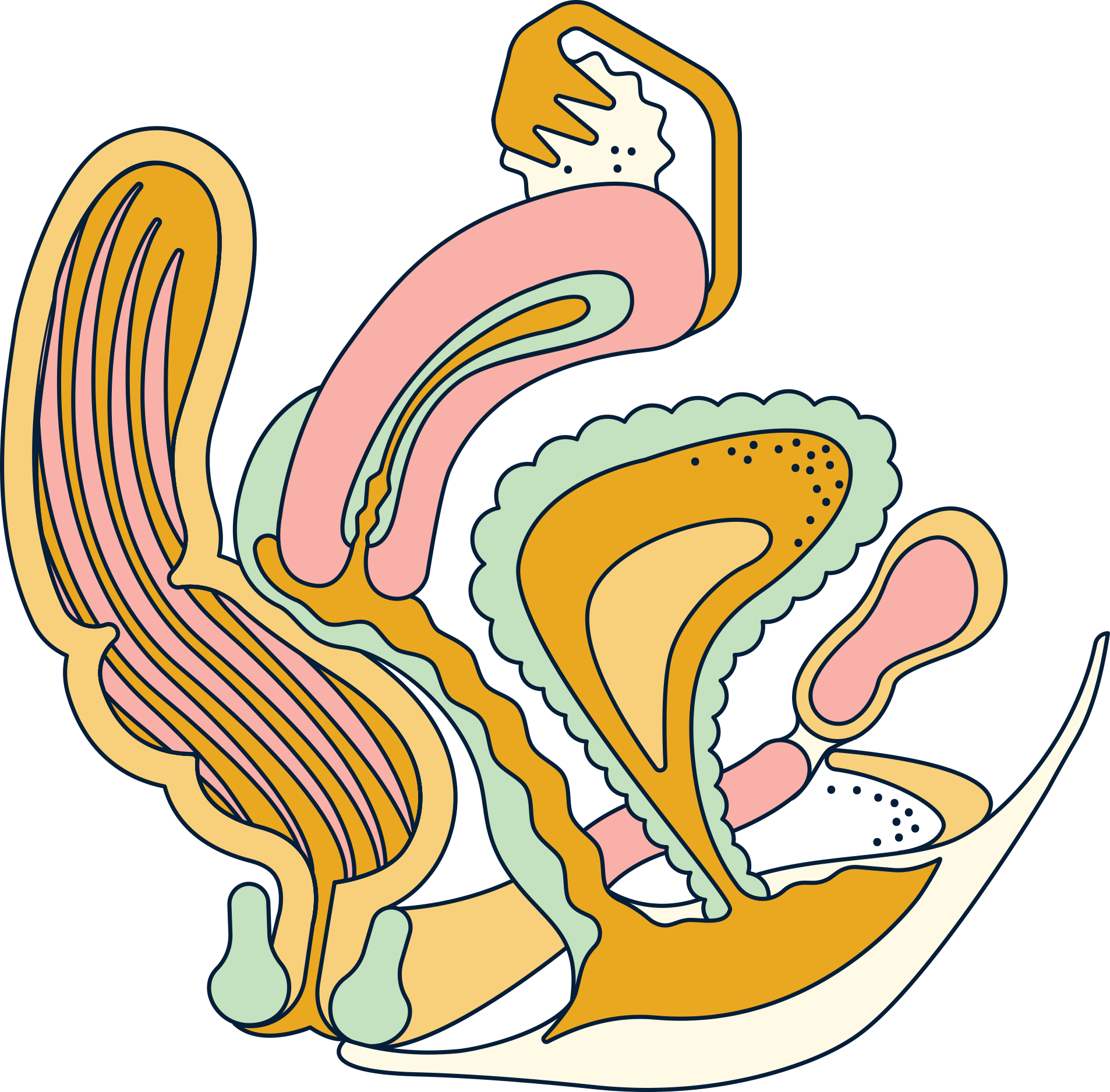
Illustrated by Erin Rommel
I think it’s fair to say that the majority of people I know have contracted an STI at some point in their lives – myself included. I had just started to sleep with an ex-boyfriend again when I got a text in the university library from the sexual health clinic informing me I had chlamydia.
Not exactly ideal, but neither was his reaction. I called him up (after going to get my meds first) and he vehemently denied giving me the infection. And this, despite the fact I hadn’t slept with anyone else and had been dating this same guy since I was 13. He repeatedly told me there was no way he could be the carrier. To say we haven’t spoken since should come as no surprise, and the fact that I am not alone in my experience is something that still needs to be addressed.
“
Pervasive stigma prevents people from going to the sexual health clinic to get tested.
In 2017 over 1.3 million tests for chlamydia were carried out in the UK. Chlamydia is essentially the common cold of STIs: it’s easy to catch, and easy to treat. While that is good news, there were also 422,147 diagnoses of sexually transmitted infections made in England that same year.
We still don’t know how many cases have been left undiagnosed, because pervasive stigma prevents people from going to the sexual health clinic to get tested. However, the government’s health protection report doesn’t cover the scenarios and the stories behind these numbers. Whilst it does state that “The impact of STIs remains greatest in young heterosexuals 15 to 24 years”, whether these people were cheated on, lied to or even sexually assaulted is not clarified.
Obviously, collecting such data requires people sharing their stories, and sexual health in the UK is still a topic that desperately needs de-stigmatising in order for open conversations to happen. Once we reach that stage, hopefully the spread of infections will slow as a result.
Of course, I understand the reluctance to get an STI check-up. It’s natural to not want to show a stranger your genitals and be asked probing questions about your sex life, all with the fear that you might actually have something looming over you the entire time.
The idea of regular STI screening needs to be introduced from an early age, and something that should feel as normal as going to a regular GP appointment. For those still struggling with the concept, however, you can get free, confidential STI tests sent straight to your door across most of the UK along with free online support through many online services.
“
It’s natural to not want to show a stranger your genitals and be asked probing questions about your sex life.
In July last year the UK government announced that Relationships and Sex Education (RSE) will become compulsory in schools in England from 2020. The current guidelines hadn’t been updated since 2000 (!) so they fail to address topics relevant to young people today such as sexting, revenge porn, consent and LGBTQIA+ identities and experiences.
This is a very positive and necessary step. In my day (i.e. about 20 years ago), sex education was mainly focussed on the logistics of heterosexual intercourse and avoiding pregnancy. But what about those who have already passed through the education system? What about adult sex ed?
Ironically, last year my sister fell victim to a scenario rather similar to my own. “We were together for nearly a year and I went to the clinic to talk about getting a copper coil fitted. Whilst I was there, the lady suggested I do an STI check. When I got back to work, I got a text saying I had chlamydia.”
After days of denying he had anything to do with the diagnosis, her then boyfriend admitted that he had been sleeping with other people. “I think I would have found out he was cheating on me eventually, but obviously the STI just saved me a lot of time. I might have not known for years that he was cheating, at least this was actual confirmation that he had put his penis in someone else, unprotected. It’s pretty offensive.”
If you are in a committed relationship in your late twenties, it’s unlikely you will be worrying about the risk of STIs or getting regular check-ups. And in theory, you shouldn’t have to. But if left untreated chlamydia can spread to other parts of the body and lead to long-term health problems such as pelvic inflammatory disease, epididymo-orchitis and infertility, despite the fact it has little to no symptoms.
In fact, according to Sexwise more than 2 in 3 women with chlamydia won’t have any obvious signs or symptoms, which often don’t show up until 3 weeks after coming in contact with chlamydia. So at the risk of sounding paranoid, should you ever really rest on your laurels when your health is at stake?

While most government issued warnings and advice on STIs in the UK and USA are targeted at the under-25s, some recent studies suggest it’s a rising problem in the elderly as well. In 2016 The Independent published an article detailing a rise in STIs diagnoses in people aged between 50 and 70.
A report from Harvard Health published in February last year makes similar claims, due to people in this age bracket avoiding “STD screening and treatment because both they and their doctors are often reluctant to raise the issue.” Other reasons include declining immune system health, dating after divorce or death of a partner and not being accustomed to using condoms.
The whole thing reeks of stigma. We are conditioned to believe that STIs are a young, promiscuous person’s problem. There is no sex education for the elderly or, for that matter, any adult sex education at all, but in a world where you can find yourself sleeping with someone by simply swiping right on your phone, the need for adult sex education is real.
“
The whole thing reeks of stigma.
It needs to be made clear that STIs aren’t just contracted by people with a lot of sexual partners. Nor are they contracted only by single, homosexual or young people. In no way am I trying to scaremonger the masses into rushing out to a nearby sexual health clinic, it’s simply some food for thought.
If we receive regular postal reminders for cervical screenings, then why not for regular STI check-ups as well? When teaching sex education in schools, having an open dialogue with the person you are in a relationship with needs to be highlighted as a crucial component of safe sex.
“
STIs are like any other infection: some are more serious than others and some can become dangerous if left untreated, but all are preventable and most are treatable or curable.
It’s not embarrassing to get an STI, and denying you have one and then passing it onto someone else definitely won’t make it disappear. STIs are like any other infection: some are more serious than others and some can become dangerous if left untreated, but all are preventable and most are treatable or curable.
Regular STI check-ups are vital to our health and there’s no reason to be ashamed of getting one… When was the last time you got tested?
Daye is launching an at-home STI testing kit... using tampons! Learn more about Daye's STI screening and join the waitlist.