Table of contents
1. Urinary Tract Infections (UTIs)
2. Kidney stones
3. Interstitial cystitis (painful bladder syndrome)
4. Bacterial vaginosis
5. Yeast infections
6. Chlamydia
7. Trichomoniasis
8. Genital herpes
9. Vaginal tears
10. Other causes of painful urination
11. Conclusion
Medically reviewed by Sarah Montagu (NPs, SRH). Sarah is a highly-qualified sexual and reproductive health nurse with 15+ years of experience.
Illustrated by Sabrina Bezerra, Erin Rommel & Maria Papazova
Painful urination, medically known as dysuria, is your body telling you that something isn't right. Unfortunately, it's not always clear what the problem is. Painful urination is a common symptom of a whole variety of conditions ranging from the irritating UTI that will clear up in a few days to more severe sexually transmitted infections and kidney issues.
To help you figure out the source of your pain, we've put together a list of the most common causes of dysuria and the symptoms that distinguish them. Just keep in mind: in almost every case, your best course of action is to seek medical advice from your GP or local sexual health clinic. The faster you see a doctor, the quicker you can figure out the cause of your pain and start treating it.
Okay, let's dive into some of the reasons you might experience painful urination.
Urinary Tract Infections (UTIs)
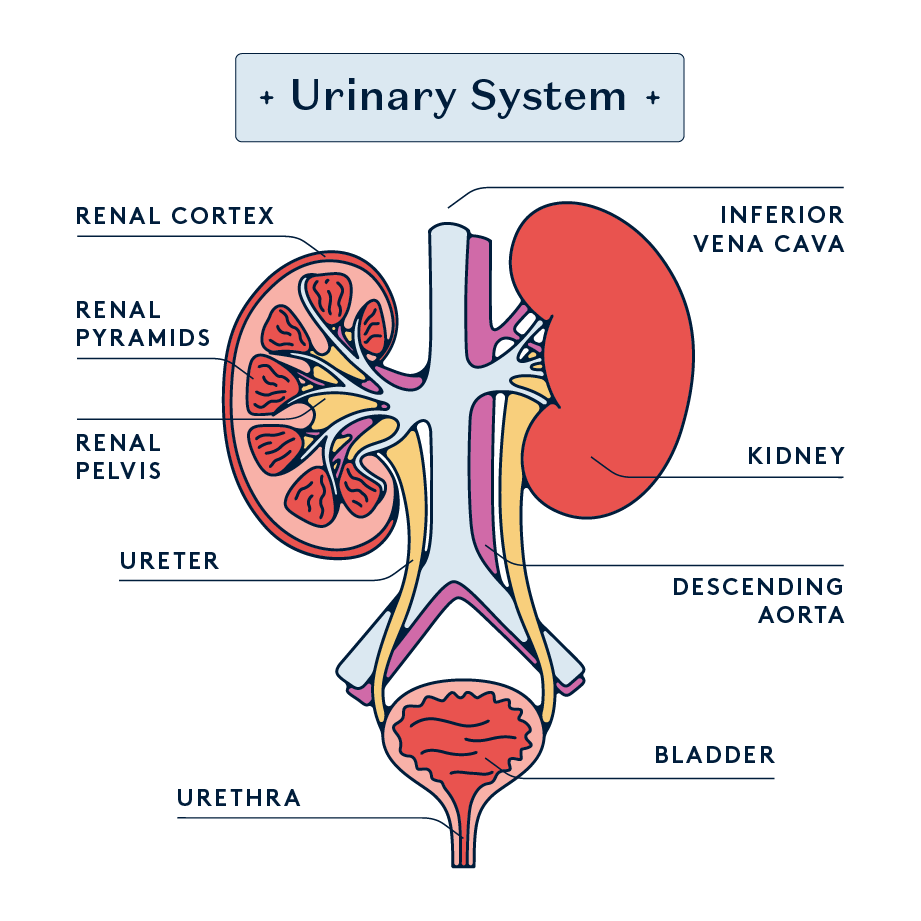
One of the most common causes of painful urination is a urinary tract infection (UTI). UTIs occur when bacteria, often from the digestive tract, enter the urinary tract through the urethra (the tube that carries urine out of the body), leading to infection anywhere in the urinary system. They can infect any part of the urinary tract, including the bladder (cystitis), urethra (urethritis), or kidneys (pyelonephritis). UTIs are particularly common in women and AFAB individuals due to their anatomically shorter urethra, which allows bacteria easier access to the bladder.
Symptoms of a urinary tract infection include a burning sensation during urination, frequent urination, cloudy or strong-smelling urine, and sometimes even blood in the urine. While some UTIs, especially mild cases, can resolve on their own, it's important to treat them promptly to prevent complications like kidney infections. Antibiotics are the primary treatment for UTIs, while over-the-counter pain relievers are also used to alleviate discomfort. A heating pad may also provide relief from pelvic or abdominal pain.
Other symptoms to look out for: peeing frequently, cloudy urine, abdominal pain, and blood in your urine.
What to do next: Stay hydrated, take over-the-counter pain relief medication, and go to your doctor to be prescribed antibiotics. If the painful urination is accompanied by fever and back pain, get in touch with a medical professional ASAP because this could indicate a kidney infection.
Kidney stones
Kidney stones are hard deposits of minerals and salts that form inside the kidneys. They can cause excruciating pain when passing through the urinary tract. Symptoms accompanying kidney stones include pain in the back, belly, or side, pain during urination, and pink, red, or brown urine. Not drinking enough water and eating a diet high in sugar, salt, and protein, and having a sedentary lifestyle can increase the risk of kidney stones.
For small stones, drinking plenty of water (about 2 to 3 litres a day) can help flush the stones out of the urinary system. Medications known as alpha-blockers can be prescribed to relax the muscles in your ureter, helping you pass the kidney stone more quickly and with less pain. For large stones, extracorporeal shock wave lithotripsy (ESWL) is used to break them down into smaller pieces that are more easily passed in the urine.
Other symptoms to look out for: Pain in the stomach, side, or back, blood in urine, fever, nausea, and vomiting.
What to do next: Contact your doctor. Make sure to get medical help immediately if the pain is very severe or if you are experiencing blood in your urine, trouble peeing, or nausea, vomiting, fever, or chills.
Interstitial cystitis (painful bladder syndrome)

Interstitial cystitis, also known as painful bladder syndrome, is a chronic condition causing bladder pressure and pain. Symptoms include pelvic pain, frequent urination, and discomfort during sexual intercourse. People with interstitial cystitis may also wake up several times in the night to pee.
Over-the-counter and prescription pain relievers can help manage bladder and pelvic pain. Pelvic floor physical therapy can also help relieve pelvic muscle tenderness, improve muscle function, and reduce pain.
Other symptoms to look out for: intense pain in the pelvic region, peeing more often than usual, finding it difficult to urinate, and blood in urine.
What to do next: Contact your doctor – they'll carry out some tests to figure out whether you're suffering from painful bladder syndrome or another condition such as bladder cancer.
Bacterial vaginosis
Bacterial vaginosis (BV) is a common vaginal infection caused by an imbalance of bacteria in the vagina. Normally, the vagina contains a balance of different bacteria, but in BV, harmful bacteria grow more than the beneficial ones. Symptoms of BV include a thin, grey, or white vaginal discharge, a fishy odour, especially after sex, and sometimes itching or burning during urination. Factors that increase the risk of developing BV include new or multiple sex partners, douching, and an imbalance in the natural bacteria in the vagina.
The treatment for bacterial vaginosis usually involves antibiotics, either in oral form or as a cream or gel applied directly to the vagina. It's important to complete the full course of antibiotics even if symptoms improve to ensure that the bacterial infection is fully cleared. An alternative to antibiotics is a lactic acid gel such as Relactagel and Balance Activ, which restores the vaginal PH and contains food for Lactobacilli (glycogen) in the hope of restoring balance to the Vaginal Microbiome. Treating with antibiotics can have side effects on your Vaginal Microbiome, commonly thrush. It is also common for BV to return after treatment with antibiotics if the Vaginal Microbiome remains unbalanced. There is also some limited evidence to support Boric acid suppositories to treat BV and thrush.
Other symptoms to look out for: Itching, a fishy smell, redness, and swelling of the vaginal area.
What to do next: Contact your healthcare provider if you suspect you have BV. Avoid self-treating with over-the-counter products before a diagnosis, as these may not be effective against BV and could mask symptoms. Remember that you can use Daye’s Diagnostic Tampon to detect BV and our pharmacy service to obtain prescription treatments and have then delivered to your door. Our highly trained nurses are available for same day consultations in case you need further support or information.
Yeast infections
Yeast infections, also known as candidiasis or Thrush, are caused by an overgrowth of a fungus called Candida, which is normally present in small amounts in the vagina. Symptoms of a yeast infection include itching, redness, and swelling of the vagina and vulva, a thick, white, cottage cheese-like vaginal discharge, and pain or burning during urination or intercourse. Factors contributing to yeast infections include antibiotic use, high oestrogen levels (such as during pregnancy), uncontrolled diabetes, and a compromised immune system.
Treatment for yeast infections typically involves antifungal medications, which can be taken orally, as a cream or suppository inserted into the vagina, or in some cases, applied topically.
Other symptoms to look out for: Pain during sex, cottage cheese-like discharge, severe redness, swelling, and irritation.

What to do next: If you experience symptoms of a yeast infection for the first time, it's advisable to consult with a healthcare provider for a proper diagnosis. If you've had yeast infections before and recognise the symptoms, you may use over-the-counter antifungal treatments, but see a doctor if symptoms persist, recur, or worsen. You can always use the Daye Diagnostic Tampon to test for yeast and thrush infections from the comfort of your home or office, using a familiar device - the Daye tampon.
Chlamydia
Another possible cause of painful urination is chlamydia. Often completely symptomless, chlamydia is a common sexually transmitted infection caused by the bacterium Chlamydia trachomatis. It can infect both men and women and can cause serious, permanent damage to a the reproductive system, potentially leading to infertility. Many people with chlamydia do not exhibit symptoms, but when symptoms do occur, they may include abnormal vaginal discharge, burning sensation during urination, pain during intercourse, and bleeding between periods.
The primary treatment for chlamydia is antibiotics, typically azithromycin or doxycycline. It's crucial for sexual partners to be treated simultaneously to prevent reinfection. Abstaining from sexual intercourse until the treatment is complete is recommended.
Other symptoms to look out for: Pain during sex, unusual discharge, and spotting between periods.
What to do next: Go to your local sexual health clinic or do an at-home STI test. Make sure to avoid sexual activity until you have received treatment.
Trichomoniasis
Sometimes painful urination is linked to trichomoniasis, a common STI caused by a parasite called Trichomonas vaginalis. It can affect both men and women, but symptoms are more common in women and people AFAB. Symptoms in women and people AFAB include a frothy, yellow-green vaginal discharge with a strong odour, discomfort during intercourse, irritation and itching of the genital area, and burning during urination.
Trichomoniasis is usually treated with a single dose of an antibiotic, most commonly metronidazole or tinidazole.
Other symptoms to look out for: fishy-smelling, frothy, thin, or yellow-green discharge, itching and soreness around the vagina, and painful sex.
What to do next: get tested for sexually transmitted infections and abstain from sex until you have received treatment.
Genital herpes
Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV), either type 1 (HSV-1) or type 2 (HSV-2). Women and AFAB individuals with genital herpes typically experience outbreaks of blisters or sores on or around the genitals, buttocks, or inner thighs. These blisters can be painful and may cause itching or burning sensations, especially during urination. Other symptoms can include vaginal discharge, swollen lymph nodes in the groin, painful urination, fever, and body aches.
Treatment for genital herpes focuses on managing symptoms and reducing the frequency of outbreaks. Antiviral medications are commonly used. These medications can be taken during outbreaks to hasten healing or continuously as suppressive therapy to reduce the likelihood of recurrent episodes.
Other symptoms to look out for: Sores, itching, headaches, muscle aches, and difficulty during urination.
What to do next: If you suspect you have genital herpes, or if you experience symptoms, it is important to consult a healthcare provider for a proper diagnosis. While there is no cure for herpes, antiviral medications can help manage the condition. These are most effective if taken early on, so do not delay seeking medical attention.
Vaginal tears
Vaginal tears, also known as perineal lacerations, are another issue that can cause painful urination. These are relatively common among women and AFAB individuals, particularly those who have recently gone through childbirth. These tears can range from minor abrasions to more significant lacerations that involve the perineal muscle and anal sphincter. Vaginal tears can also occur due to sexual activity, especially if there is insufficient lubrication, or as a result of injury. Symptoms of a vaginal tear include pain, bleeding, discomfort during urination, and, in more severe cases, incontinence of gas or stool.
The treatment for vaginal tears depends on their severity. Minor tears may only require pain relief and proper hygiene to prevent infection, while more significant lacerations might need surgical repair. In cases of childbirth-related tears, repair is usually done immediately post-delivery.
Other symptoms to look out for: Swelling, bruising, and increased pain or discomfort, which could indicate infection or more severe injury.
What to do next: If you suspect a vaginal tear, especially if you experience severe pain, excessive bleeding, or signs of infection, it is important to seek medical attention. For minor tears, maintaining cleanliness, applying cold packs for swelling, and using over-the-counter pain relief can be helpful. Avoid penetrative sex and using tampons as this can make the symptoms worse.
Vaginal tears can be a result of “rough sex” which isn’t always consensual. For support, if you have been sexually assaulted or raped, you can contact Rape Crisis on 0808 500 2222.
You can find your nearest Sexual Assault Referral Centre here. You can also find support at your local GP, voluntary organisations such as Rape Crisis, Women's Aid, and Victim Support, and you can report it to the police (if you choose) here.
Other causes of painful urination
While we've already covered many of the common conditions that can make you feel pain while you pee, don't rule out the following possibilities:
- Chemical Irritants: Exposure to chemicals found in products such as soaps, body washes, vaginal sprays, scented toilet paper, douches, and contraceptive foams or spermicides can irritate the urethra and cause painful urination.
- Allergic Reactions: Allergies to certain materials, such as latex (found in some condoms or diaphragms), also chemicals found in some period care products, can cause localised irritation leading to pain during urination.
- Medications: Certain medications, particularly those used in chemotherapy or radiation therapy, can irritate the bladder and urethra.
- Bladder Cancer or Stones: Although less common, bladder cancer or bladder stones can cause irritation and discomfort during urination.
- Pelvic Inflammatory Disease (PID): In women and AFAB folks, an infection of the reproductive organs can cause pain during urination as part of a broader set of symptoms.
- Urethral Stricture: A narrowing of the urethra due to scar tissue, often resulting from injury or infection, can restrict urine flow and cause you to experience pain while peeing.
Conclusion
Painful urination can be an indicator of a wide range of issues, ranging from urinary tract infections to chronic pelvic pain conditions, kidney stones, or even sexually transmitted diseases. While the cause is often a simple urinary tract infection, it's still important to seek medical treatment just in case it's something worse.
Concerned about STIs? Don't worry – we've created a world-first STI test that you can take at home using just a special tampon. No uncomfortable swabs or urine sample necessary! Just order your STI test kit, find out your results, and access treatment consultations with specialist gynaecologists, nurses, and fertility experts today.






