Table of contents
1. Why Do Migraines Impact Women More Than Men?
2. Can Some Women Experience Migraines Exclusively Around Their Periods?
3. Is There A Link Between Severe Period Pain and Migraines?
4. Key Tips For Coping With Migraines
Illustrated by Sabrina Bezerra, Erin Rommel & Valko Slavov
If you’ve experienced even one migraine in your life, you’ll likely never forget the excruciating, all-consuming pain and discomfort; and if you have a womb, you may have noticed migraines appearing at a particular time of the month.
“A migraine is a specific type of headache characterised by intense, pulsating pain, often accompanied by other symptoms such as nausea, vomiting and sensitivity to light and sound,” says Dr Amira Bhaiji, Internal Medicine Physician at Chelsea and Westminster Hospital (who also sits on Daye’s Advisory Board).
To my knowledge, I’ve never had a migraine; and the fact that I wrote ‘to my knowledge’ proves that I almost certainly haven’t. If it’s a migraine – you know. “What distinguishes migraines from other types of headaches, such as tension or cluster headaches, is their severity and the presence of [the aforementioned] additional symptoms,” Bhaiji explains. “Migraines can typically last for hours to days and can significantly disrupt a person’s daily life.”
Too often, migraines are underserved and dismissed by healthcare professionals as ‘just a headache’. Couple this with the fact that migraines affect women more than men and the ever-present gender pain gap, which frequently sees women’s pain written off as being of little importance; and the result? AFAB individuals are likely experiencing crippling migraines without getting the help they need.
Enter, Quash: A new migraine support service that prioritises personalised migraine treatment plans. Focusing on the latest evidence about what works best for individuals, Quash prescribes from a vast range of symptom-relieving medications for those who experience four or fewer migraines per month.
Ultimately, Quash wants to put an end to the routine dismissal and misdiagnosis of migraines; and, through its personalised care which is tailormade for each person, it also calls attention to a unique phenomenon affecting AFAB individuals – that of the link between migraines and periods.
So, without ado, let’s take a deep dive into the (painful) relationship between menstruation and migraines.
Why Do Migraines Impact Women More Than Men?
First, some stats.
“Research has shown that women are three times more likely than men to have migraines, and they occur more frequently than men’s, last longer and make daily activities more difficult to deal with,” says Dr Samantha Wild, Clinical Lead for Women’s Health and GP at Bupa Health Clinics
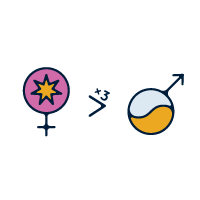
Indeed, in the US alone – according to the Migraine Research Foundation – 18% of women are impacted by migraines; compared to 6% of men.
Dr. Betsy A.B. Greenleaf, DO, FACOOG (Distinguished), FACOG, who also called attention to this stat, explains that hormonal fluctuations play a significant role in this gender disparity. “Oestrogen, a hormone that regulates the menstrual cycle, is believed to have an influence on the occurrence of migraines,” Greenleaf says. “Fluctuations in oestrogen levels, such as those experienced during menstruation, pregnancy and menopause, can trigger migraines in certain women.”
Can Some Women Experience Migraines Exclusively Around Their Periods?
In short: Yes.
“Before your period, the amount of oestrogen in your body naturally drops,” says Wild. “When this happens, it can leave you more vulnerable to developing a migraine.
“When migraines only happen around this time, they’re known as ‘menstrual migraines’, and the symptoms tend to be more severe than migraines at other times of the month,” Wild continues. “They’re also more likely to return the following day.
Is There A Link Between Severe Period Pain and Migraines?
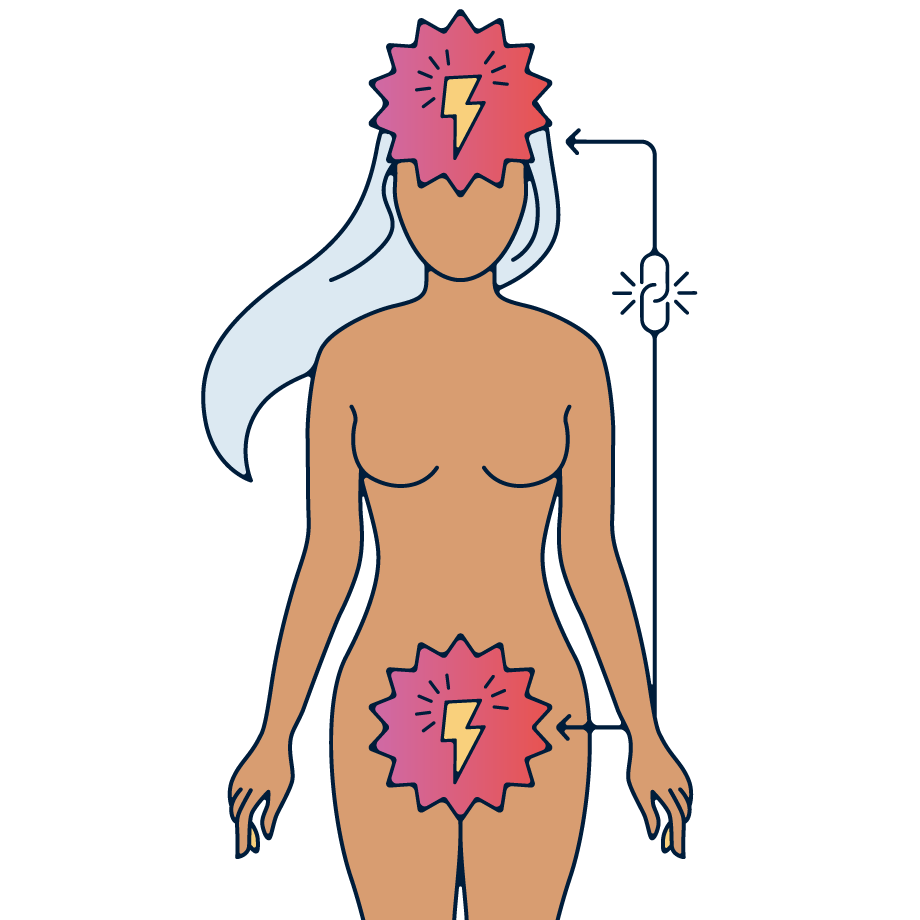
“The link between severe period pains and migraines, particularly through the hormone prostaglandin, is an interesting area of study,” muses Greenleaf. “Prostaglandins play a role in the uterine muscle contractions that help to shed the uterine lining, which can cause pain. Elevated prostaglandin levels have also been implicated in menstrual migraines.”
“This connection is complex,” agrees Bhaiji, who, too, acknowledges the importance of prostaglandins in the interplay between acute period pain and migraine onset. “Elevated prostaglandin levels can also lead to increased sensitivity to pain, and this can trigger or worsen migraines in some women. This interplay of hormones and pain sensitivity can make the relationship between period pain and migraines more pronounced in some individuals.”
Key Tips For Coping With Migraines
As well as being personally painful and debilitating, migraines can impact the UK economy due to the ways in which they affect productivity in the workplace. The Migraine Trust points out: “It is estimated people in the UK lose a total of 43 million days from their work and education each year because of migraine.” That’s a hell of a lot of days lost to something that, too often, gets dismissed.
So, really, it’s in everyone’s interest to address this issue. And, on that note, once again: enter, Quash – who have highlighted four key tips for migraine care.
- Get help
- It’s important to state initially that over-the-counter painkillers can be transformational in easing pain. “First, try [OTC] painkillers like paracetamol and ibuprofen if they’re suitable for you,” says Wild. “If migraines make you feel nauseous or sick, you can also ask for anti-sickness medication from your pharmacist, too.”
- But it’s important not to purely rely on over-the-counter painkillers; always go to your GP as well. In severe cases, they might even be able to refer you to a neurologist or headache specialist.
- Plus, as Greenleaf points out: “It is highly recommended to have migraines assessed by a healthcare professional, as not all headaches are migraines. It is crucial to rule out other potentially serious conditions.”
2. Keep a headache diary
- “[This will help you] track potential triggers like foods, stress, sleep patterns or hormonal changes,” says Bhaiji.
- Plus, any prescriber – Quash or otherwise – will ask usually ask you for details of your symptoms. A diagnosis from a GP is tricky without these details; so keep a log of frequency, pain levels and any medication you’ve already tried.
- You could do this on your phone, through an app like Migraine Buddy or – if you’re old school like me – in a physical notebook.
3. Watch the painkillers
- They can be very useful – but too many might have the opposite effect.
- “Overusing over-the-counter pain medications can lead to medication overuse headaches,” says Bhaiji. “It’s essential to use migraine-specific medications as prescribed by a healthcare professional or any natural remedies that work for oneself.”
4. Research your options
- Quash is emphatic that there is simply no ‘one-size-fits-all’ for migraine; and the more informed you are about potential solutions and coping strategies, the more able you will be to seek help.
- Ask your Quash prescriber or your GP to talk you through the range of medications available to you and your specific life circumstances, any potential risks and benefits, and when each is recommended.
- Quash also recommends perusing patient reported knowledge base Stuff That Works to learn about what has been effective for other migraine sufferers. Always talk about anything you’ve found with a healthcare professional, rather than self-diagnosing and self-treating; but it’s a useful place to start to know your options.
As Bhaiji concludes: “The impact of migraines on women’s lives extends far beyond the pain and discomfort during an attack. It can influence their career, relationships and overall quality of life. This underscores the importance of recognising the unique challenges women face when dealing with migraines and the need for tailored treatments and support in the realm of women’s health to mitigate these challenges and improve their overall well-being.”
Couldn’t have put it better myself.






