Table of contents
1. Primary dysmenorrhea
2. Secondary dysmenorrhea
3. Other factors that contribute to painful periods
4. Managing your period pain
Medically reviewed by Sarah Montagu (NPs, SRH). Sarah is a highly-qualified sexual and reproductive health nurse with 15+ years of experience.
Illustrated by Sabrina Bezerra, Erin Rommel & Maria Papazova
If you have a period, it's almost certain that you've experienced period pain. According to one survey, 96% of 16-40 year old UK women have experienced period pain, and one in five are estimated to feel no relief from existing treatments such as NSAIDs or hormonal birth control pills.
Period pain may include a cramping, aching pain in your abdomen, pain in your lower back, hips, and thighs, feelings of pressure in your abdomen, and even other symptoms like headaches and nausea. For some women and AFAB folks, the severe pain means that they have to miss work or school; those who do go to work with period pain are estimated to lose 9 days worth of productivity per year.
But what causes period cramps in the first place? Let's take a closer look at dysmenorrhea (the technical term for period pain) and why it happens.
Primary dysmenorrhea
Primary dysmenorrhea refers to period pain that's not associated with another health condition. It's basically a diagnosis of exclusion – if there's no issue such as endometriosis or pelvic inflammatory disease (PID) causing the pain, you'll be diagnosed with primary dysmenorrhea.
Just because primary dysmenorrhea isn't associated with an underlying medical condition doesn't mean it's no big deal. In fact, primary dysmenorrhea can be extremely painful and distressing.
What exactly causes the painful menstrual cramps?
Further research into the causes of primary dysmenorrhea is needed, but scientists currently think that it's linked to hormone-like chemicals called prostaglandins. These chemicals have a range of different purposes within the body, but one of their key roles is to cause the uterus to contract and relax over and over in order to expel the uterine lining.
When the uterus contracts, blood flow and oxygen levels are disrupted in the muscles, so metabolic byproducts and other chemicals such as lactic acid build up within the uterine muscle tissue. These chemicals can activate nerve fibres that transmit pain signals to the brain. The sensation of pain is essentially the body's way of signalling that the tissue is under stress. To make matters worse, prostaglandins also make the nerve endings in the uterus more sensitive to pain, effectively lowering the pain threshold so that you'll feel it even more!
While prostaglandins are absolutely essential in the body, having an excess of them might be the cause of primary dysmenorrhea. There's evidence that people who experience higher levels of period pain also have higher concentrations of prostaglandins in their body. This is partly why taking nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce menstrual cramps; NSAIDs block the effects of prostaglandins in the uterus.
Secondary dysmenorrhea
Secondary dysmenorrhea can feel the same as primary dysmenorrhea, but it's caused by an underlying pelvic condition. The pain might occur throughout the cycle, before menstruation begins and after it ends, but might also be exacerbated during the menstrual period. Often, a person may have had years of painless periods before its onset.
Here are a few of the conditions that are associated with secondary dysmenorrhea.
Endometriosis
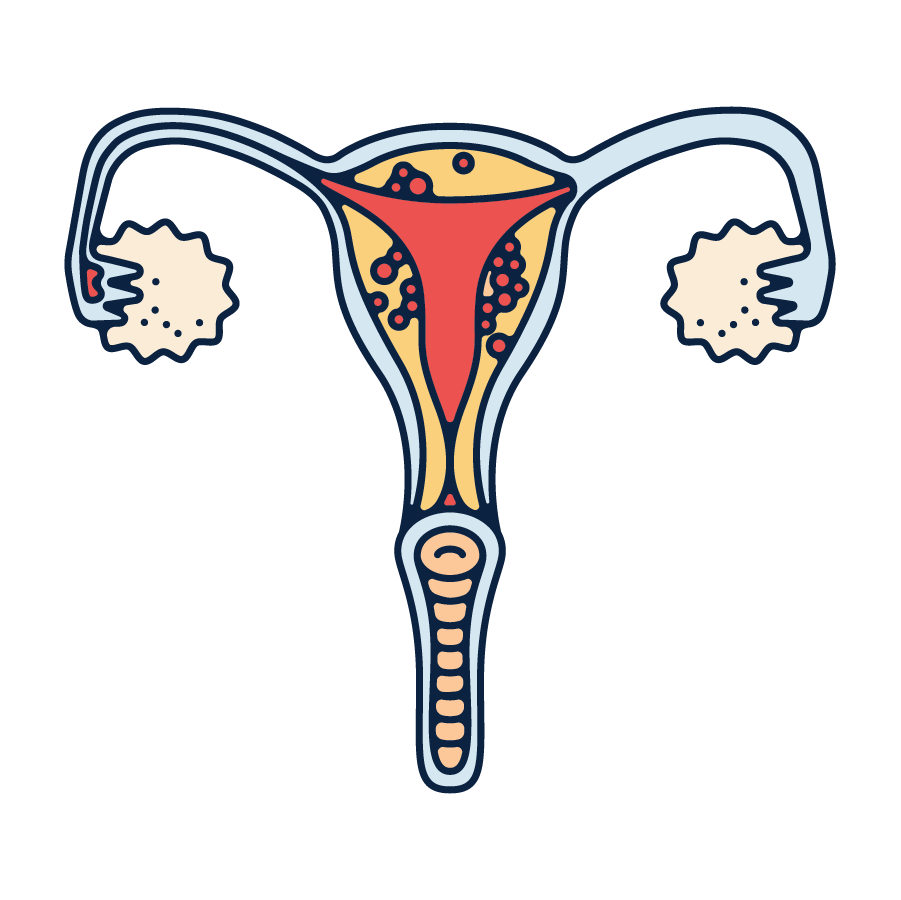
Endometriosis is the most common cause of secondary dysmenorrhea. This is a condition where cells similar to those in the lining of the uterus grow in other parts of the body, such as the fallopian tubes, ovaries, and bowels. Just like the uterine lining, these cells build up every month and then shed during your period. However, unlike the uterine lining which is expelled through the cervix and vagina each month, there's no way for these cells to exit the body. As a result, they build up over time, causing inflammation, pain, and scar tissue. Extremely heavy and painful periods are one of the common symptoms of endometriosis.
Uterine fibroids
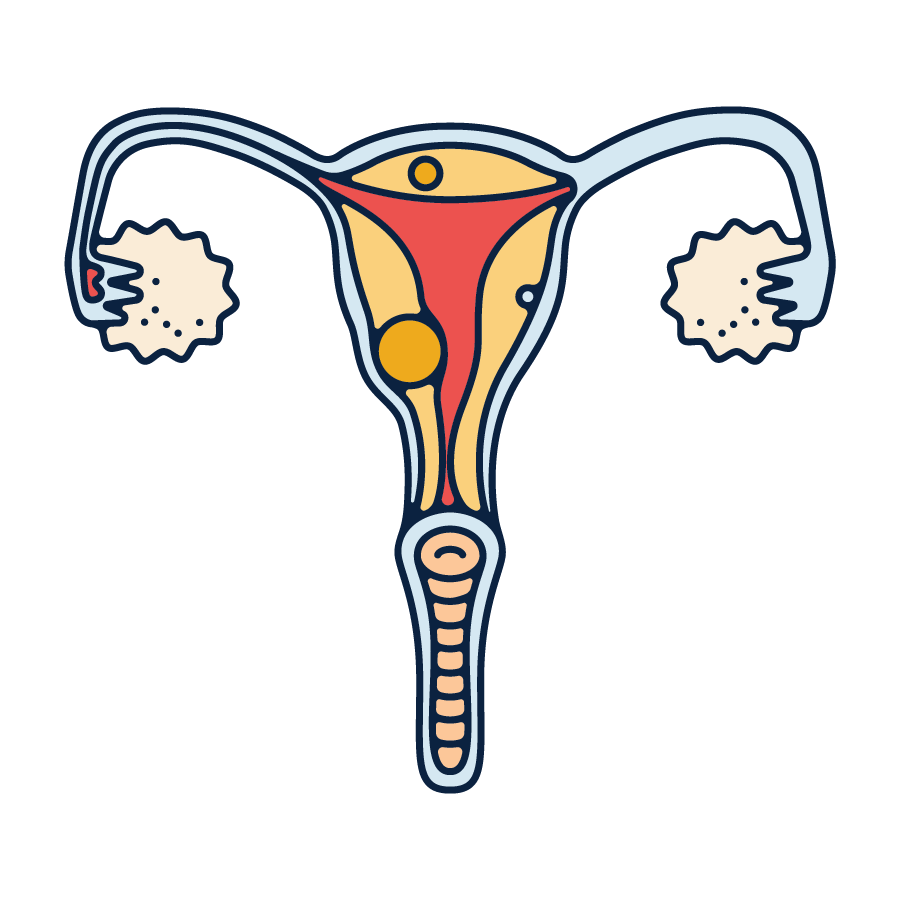
Fibroids are non-cancerous growths of muscle and fibrous tissue that develop in or around the uterus. Although they may sound scary at first, uterine fibroids are extremely common and usually don't cause symptoms. In fact, two in three people with uteruses will develop a fibroid during their lifetimes, and only around a third of those will experience any symptoms at all.
Painful periods are one of the more common symptoms in people who are symptomatic at all. Fibroids can worsen painful cramps for a number of reasons. Firstly, the fibroid puts additional pressure on the lining of the uterus, surrounding organs and tissues. Secondly, they can create additional surface area in the uterus which means more lining must be shed during menstruation. This means you're likely to experience a heavier flow and bigger clots. The uterus has to work overtime to push this additional menstrual fluid out of the body, so you'll experience more contractions and more pain.
Pelvic inflammatory disease (PID)
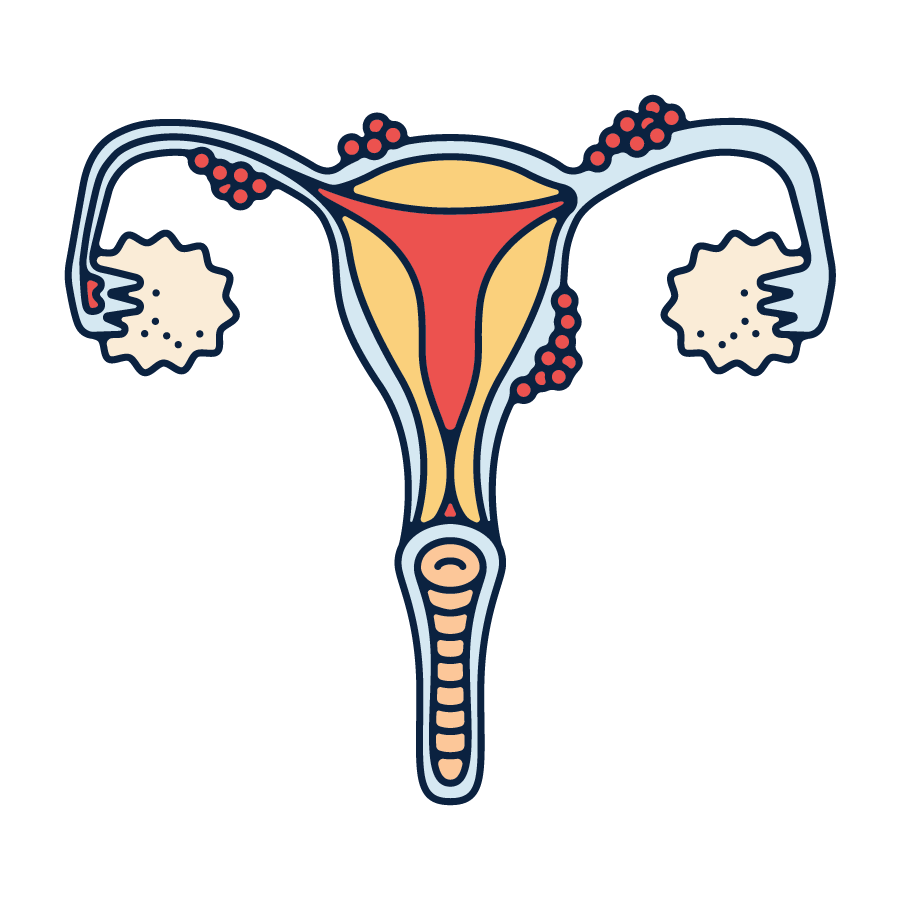
Pelvic inflammatory disease is the name for an infection of the reproductive organs which is usually caused by a bacterial infection that has spread from the vagina or cervix. Often this can be caused by sexually transmitted infections such as chlamydia, gonorrhea, or mycoplasma genitalium.
Painful periods are just one symptom of PID, alongside pain during sex, intermittent pelvic pain, unusual vaginal discharge, bleeding in between periods or after sex, and pain while urinating. Your periods may also become heavier and last longer if you have pelvic inflammatory disease.
Adenomyosis
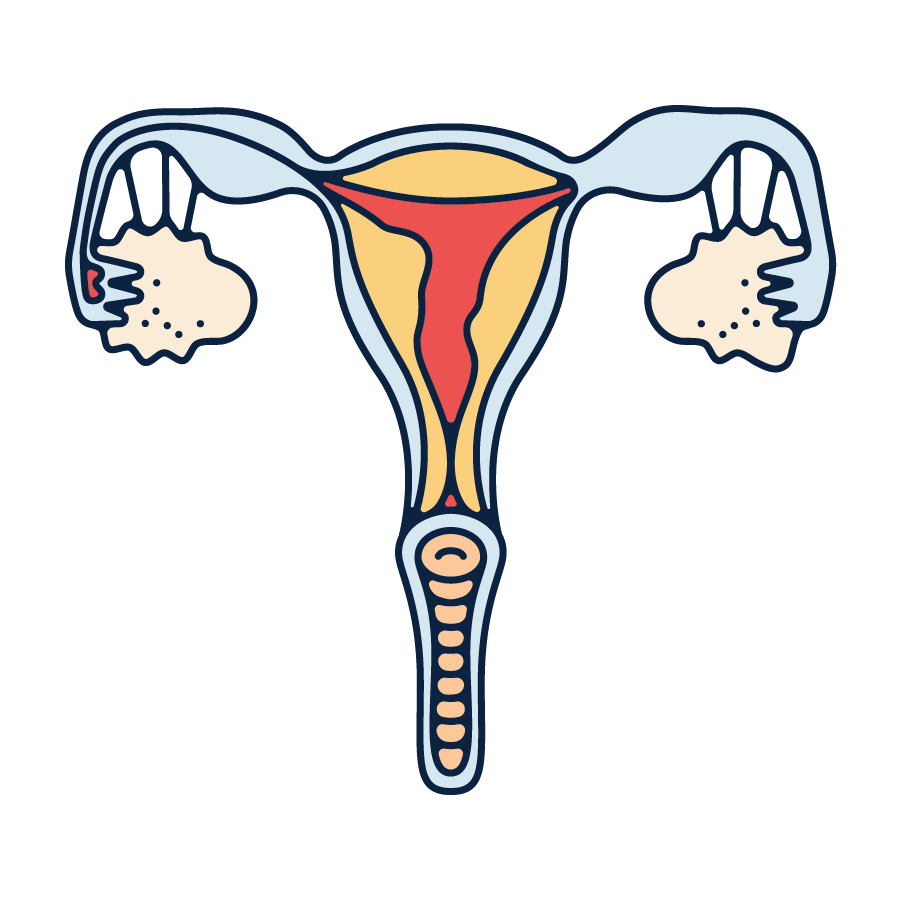
Adenomyosis is a condition where the endometrial tissue lining the uterus starts to grow into the muscular wall. This can cause the uterus to enlarge to up to triple its usual size.
Adenomyosis can cause more severe period pain as well as heavier bleeding. This is in part because the tissue growing into the uterine muscle disrupts the normal functioning of the muscle fibres. This can lead to abnormal and often painful uterine contractions. The enlarged uterus can lead to increased pressure and pain in the pelvic area. Moreover, during your period, the endometrial tissue growing in the muscle also tries to break down like the normal uterine lining does – this can lead to increased inflammation and pain in the short term. In the long term, it can cause scarring within the muscle, which also exacerbates the pain.
Uterine Polyps
Growths of endometrial tissue that attach to the inner wall of the uterus and extend into the cavity are known as uterine polyps. These are usually non-cancerous but they can contribute to more painful periods. Like uterine fibroids, their presence means more endometrial shedding and local inflammation within the uterus which can cause more pain. Larger polyps can also cause cramping pain outside of your period as the uterus tries to expel them.
Ovarian cysts
Ovarian cysts are fluid-filled sacs or pockets within or on the surface of an ovary. While many women develop ovarian cysts at some point, they often cause no symptoms and go away on their own. However, when symptoms do occur, they can contribute to secondary dysmenorrhea. These cysts can cause pelvic pain, especially during menstruation, as they may put pressure on the reproductive organs.
Intrauterine devices (IUDs)
Intrauterine devices are a form of long-term birth control inserted into the uterus. While highly effective for contraception, they can sometimes cause secondary dysmenorrhea, especially during the first few months after insertion. The presence of a foreign object in the uterus can lead to increased menstrual cramps and discomfort, along with heavier bleeding.
Whether your menstrual cramps worsen after getting an IUD often depends on the type of device you choose. A hormonal IUD often makes periods lighter or makes them go away altogether. In contrast, a copper IUD can often make heavier and painful menstrual periods more likely.
Inflammatory bowel disease
Inflammatory bowel disease (IBD), which includes conditions like Crohn's disease and ulcerative colitis, is characterised by chronic inflammation of the gastrointestinal tract. While primarily affecting the intestines, IBD can also have implications for menstrual health and contribute to secondary dysmenorrhea. The inflammation associated with IBD can exacerbate pelvic pain and discomfort during menstruation. It can also contribute to irregular menstrual cycles.
Other factors that contribute to painful periods
Lifestyle factors can also have a significant impact on painful menstrual periods
Diet
Studies have shown that diet can have a significant impact on period pain. For example, one study carried out in Iran found that women who ate a diet high in sugar, sweets, desserts, salty snacks, fruit juices, tea, coffee, and added fats were more likely to suffer from dysmenorrhea than those who ate less junk food. An Italian study found that women who ate more fruit, fish, and eggs were less likely to suffer from menstrual pain, while another small study from the USA found that following a low-fat vegetarian diet for two menstrual cycles reduced the intensity and duration of period pain as well as the duration of premenstrual syndrome.
These studies tend to look at overall diets rather than particular foods, but on the whole it's clear that eating foods that are high in fibre and magnesium can help reduce pain by reducing the body's synthesis of prostaglandins. Think: leafy green vegetables, nuts, seeds, whole grains, and fatty fish to get your beneficial omega-3 fix (you can also take this in the form of dietary supplements).
Smoking
Smoking cigarettes is another of the risk factors for increased period pain. One study carried out in Australia followed over 9000 young women throughout a 12 year period and found that 29% of smokers suffered from period pain compared to 23% of non-smokers. In fact, smokers were 40% more likely to experience ongoing pain throughout the whole study. Some of the women who stopped smoking during that period saw reduced menstrual pain, but their pain levels were still higher than those who had never smoked.
We still don't know exactly how smoking contributes to menstrual cramps, but it may be to do with its ability to narrow blood vessels and reduce oxygen flow. The smoke may irritate the lining of the uterus, damage the ovaries, or even affect your hormones. While further research is still required to find out the exact mechanisms, it's clear that cigarettes are deeply harmful to your reproductive organs and the rest of your body's health.
Alcohol
While some people might be tempted to reach for a glass of wine to dull the cramps, it can actually cause more pain and increase the symptoms of PMS. The same Italian study mentioned earlier found that women who drank less wine were less likely to suffer from dysmenorrhea. Why? Alcohol lowers your magnesium levels and increases prostaglandins (so your uterus contracts more intensely), while also having a dehydrating effect which can worsen menstrual cramps. Meanwhile, heavy drinking can cause changes in hormone levels, potentially disrupting ovulation and causing irregularities in your cycle.
Managing your period pain
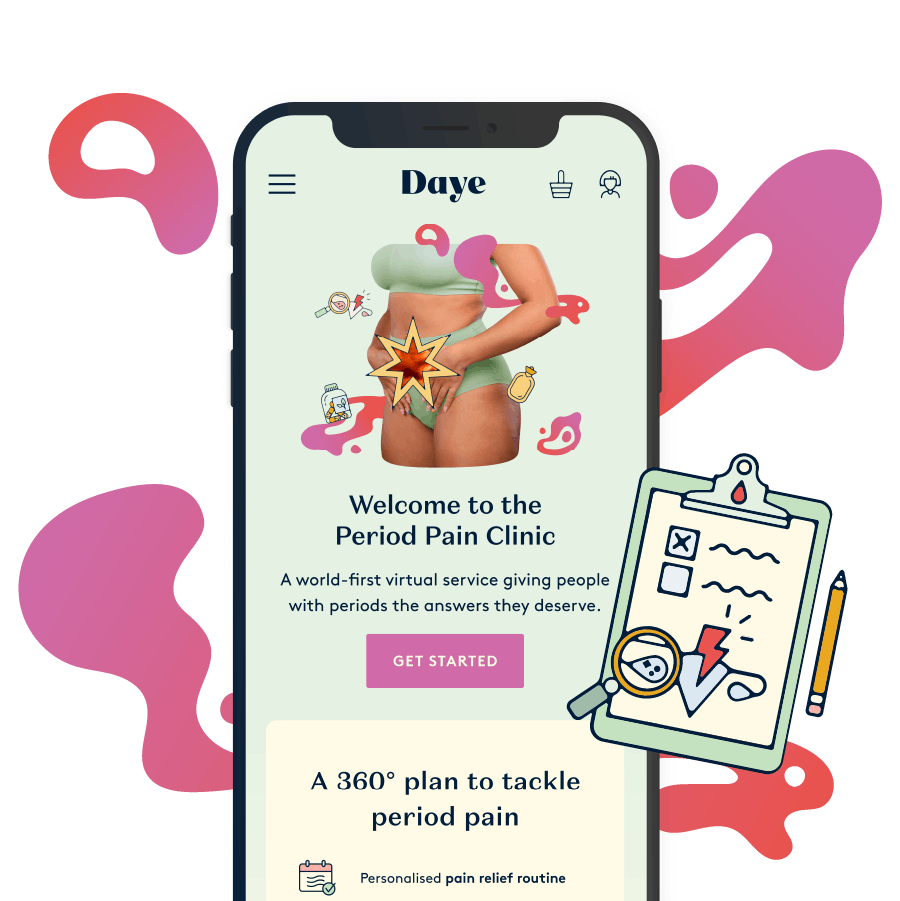
Dysmenorrhea (both primary and secondary) has a huge impact on the lives of people who menstruate, but fortunately there are ways to manage it. Here at Daye, we know just how often women, girls, and AFAB folks have their pain dismissed by doctors as 'just a period', and we're here to change that. Our Period Pain Clinic is designed to help you find out the causes of your menstrual pain and access personalised treatment plans developed with specialists. Want to give it a go? Get started with your free personalised report by filling out our period pain questionnaire.






