Table of contents
1. Vaginal thrush symptoms aren’t fun, to say the least; but, regrettably, thrush is common.
2. Yes, you did read that right. Frequent, recurring or even constant vaginal thrush sounds like the stuff of gynaecological nightmares; but it happens.
3. So: why does three-year long recurrent thrush happen?
4. And there are some at-home remedies you can try, too: like Daye’s upcoming Vaginal Microbiome Screening (VMS).
Written by Izzie Price
Illustrated by Sabrina Bezerra Erin Rommel
On the one hand, there are some pretty great elements: the vagina’s ability to self-cleanse, for example. Vaginas are amazing; but they can come with their own set of complications (at best) and uncomfortable, painful issues (at worst). One such issue? Vaginal thrush.
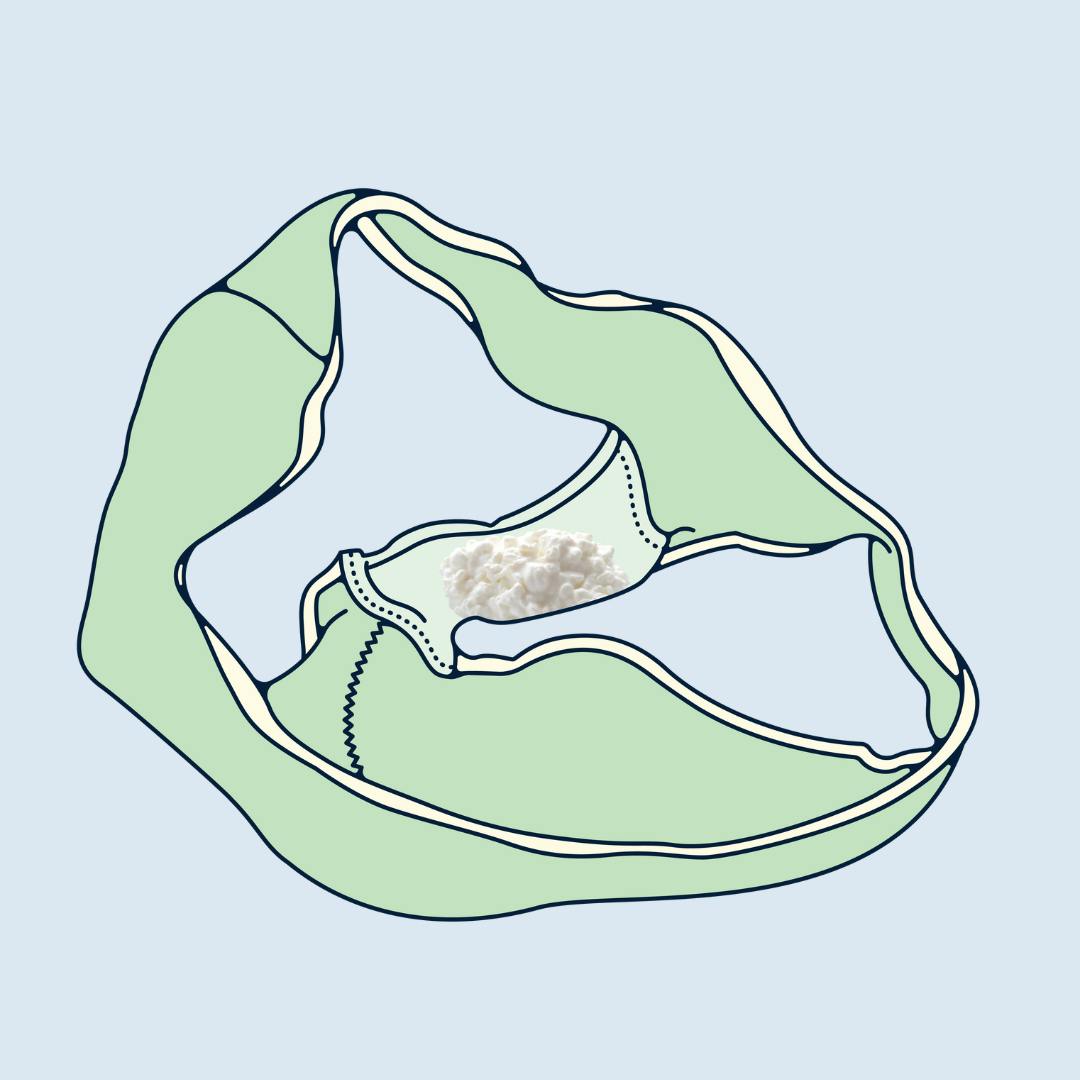
Show me someone with a vagina who’s never suffered from vaginal thrush and I’ll be begging them for their secret within two minutes. Which of us hasn’t been there? Itching that feels like it can only be soothed by running ice cubes back and forth over the vulva; a twanging pain that may as well be someone stabbing a needle repeatedly into the vaginal wall as you walk upstairs; a thick, cottage cheese-like vaginal discharge; the list goes on.
Vaginal thrush symptoms aren’t fun, to say the least; but, regrettably, thrush is common.
In fact, around 75% of people will contract thrush during their lifetime, says Claire Bailey: Consultant Gynaecologist at The Vulval Clinic.
“Thrush refers to an infection caused by the fungus (yeast) Candida,” Bailey tells me. “Candida normally lives on the skin and in the mouth, intestines and vagina without causing any problems or symptoms. Numbers of the organism are kept under control by the surrounding bacteria. If there is an imbalance of bacteria, however, it is possible for the Candida species to increase in number.
“When there is an overgrowth of the fungal organism, Candidiasis or ‘thrush’ occurs,” Bailey continues. “This happens most commonly in the vagina.”
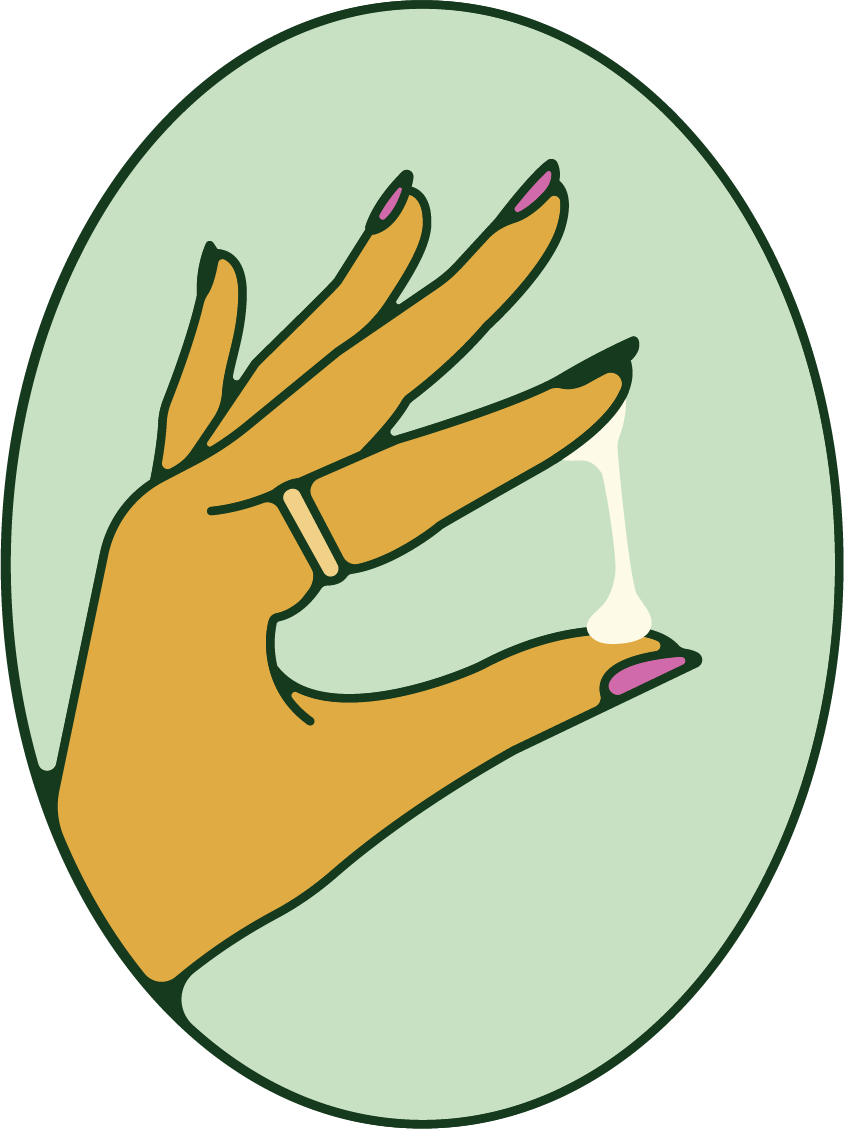
Chances are, you’ll be familiar with vaginal thrush symptoms – but Dr Sam Wild, Women’s Health Clinical Lead for Bupa Health Clinics, points out that thrush may not always appear in the way we’d expect. “Sometimes, vaginal thrush has no symptoms, so you might not realise you need treatment,” Wild warns. “However, it can manifest in itching or soreness in or around your vulva, along with experiencing thick, white vaginal discharge. You may also find sex painful, along with peeing; [and] thrush can also affect [all] genders in other skin areas, like between your fingers and in your armpits or groin.”
It seems somewhat superfluous, then, to say that thrush isn’t a condition anyone wants to get. But if you get it once or twice for a few days – or an episode that “clears up within 7 to 14 days”, as Wild says is usual – think yourself lucky: because it’s possible to get it for up to three years or more.
Yes, you did read that right. Frequent, recurring or even constant vaginal thrush sounds like the stuff of gynaecological nightmares; but it happens.
“Thrush is usually easily treated with over-the-counter medication,” says Bailey. “[But] it is possible for thrush to be an ongoing problem with symptoms lasting more than three years. In such cases, it is important to see your doctor to confirm the diagnosis.
“This can be done by taking a swab from the vagina,” Bailey goes on. “Your doctor can then determine whether the Candida infection is recurrent (being effectively treated but recurring soon after treatment) or is resistant to traditional first line treatments”: which include “antifungal creams and vaginal pessaries”, Bailey says. “Recurrent thrush is defined as four or more episodes in 12 months.”
“
If you’re struggling with recurring thrush – you’ve had it more than four times in the last year – speak to a GP or a sexual health clinic.
So: why does three-year long recurrent thrush happen?
“It’s not always clear why some people suffer from recurring thrush,” muses Wild. “However, it’s thought that your body’s individual bacteria levels and immune system may contribute to a higher chance of developing recurring thrush.”
When it comes to vaginal thrush treatment for when you’ve struggled with thrush for three years or more, it’s vital to seek professional advice. “If you’re struggling with recurring thrush – you’ve had it more than four times in the last year – speak to a GP or a sexual health clinic,” Wild emphasises. “[They] will help to check whether there’s something specific [that’s] leading to recurring thrush – for example, having your period or any medications or underlying illnesses. Once any other potential cause has been established, you’ll be given personal recommendations on how often you should use thrush treatment.”
Bailey agrees. “Occasionally, routine antifungals do not work,” she explains of the typical “first line” treatment. “Most thrush infections are caused by the organism Candida albicans which responds well to regular antifungals such as Clotrimazole and Fluconazole. Sometimes, a different Candida is responsible, in which case alternative antifungals may be more efficacious”; but you’ll need to see a healthcare professional in order to determine this. “Prophylactic oral treatment, often taken for six months, can be very useful in managing recurrent Candidiasis,” Bailey adds. “Speak with your doctor.”

And there are some at-home remedies you can try, too: like Daye’s upcoming Vaginal Microbiome Screening (VMS).
You know the Daye tampons you’ve been using and loving? Well, now you can send a used tampon back to Daye’s lab: and it’ll be analysed for vaginal microbiome imbalances. Via online results, it’ll confirm if you have thrush in the first place (ideal if you don’t have any symptoms); but it’ll also tell you if your microbiome is disrupted, which can often be a precursor to thrush.

In the meantime, Bailey suggests that you “wipe front to back after going to the loo as this stops transfer of Candida from around the anus to the vagina”, and that “if symptoms occur around the time of your period, use of tampons rather than [pads] may help”; while Wild posits “after washing, always make sure you dry yourself thoroughly” and that you “be sure to wear breathable cotton underwear that isn’t too tight”, together with making sure a previous vaginal thrush infection has fully cleared up before you have sex.
And one crucial vaginal thrush treatment that crops up again and again (and again): leave your vagina alone. “Swap out perfumed soaps or shower gels for water”, Wild implores; while Bailey states: “Do not overwash [or] douche the vagina”.
So if you’ve been struggling with vaginal thrush symptoms for more than three years: don’t despair. There are vaginal thrush treatments out there: just make an appointment with a healthcare professional (and get your vagina screened, whether via Daye’s VMS or otherwise) and go from there.
Relevant Products
See our Founder’s results!
Wondering what we test for, and what results look like? Enter your email below and Valentina, our Founder, will send you her screening report.
By entering your email above you agree to receive marketing emails and promotions from Daye.