Table of contents
1. A Look Back: STI Testing in The Past
2. How At-Home STI Testing Changed Everything
3. Improving STI Tests For Better Treatment and Increased Uptake
4. The Role of E-Technology in Enhancing STI Testing
5. The Future of STI Testing: Challenges and Opportunities
Written by Izzie Price
Medically reviewed by Sarah Montagu (RN DFSRH, BSc)
Illustrated by Maria Papazova
We won’t beat around the bush – sexually transmitted infection (STI) rates are soaring.
Scaremongering isn’t our thing (in fact, we hate it); but, to put it bluntly, some things are serious and need addressing – STI rates being one of them.
There’s been a 76% increase in rates of syphilis and a 36% rise in cases of chlamydia in England, and sexual health services in England and Wales are seeing 'unprecedented increases in demand'; all of which means access to STI tests is more important than ever.
The news is bleak; but the glimmer in the darkness is that, fortunately, innovation in STI screening technology is helping healthcare rise to the challenge. At-home STI test kits help people check for infections from the comfort of their own homes, access quick and easy treatment and get confidential advice about STI prevention.
Let's take a closer look at how innovation in at-home STI screening is changing the game – making sexual health management easier (especially at a time when STIs are on the rise) and more comfortable for women and AFAB folks.

What you'll learn:
- How STI testing has evolved from clinic-only to at-home options
- Latest innovations in testing technology, including tampon-based sampling
- Why digital healthcare is transforming sexual health management
- The future of STI screening and what it means for you

A Look Back: STI Testing in The Past
To understand why innovation in sexual health is so important, consider how STI testing worked in the past. Prior to advancements in medical technology and public health initiatives, individuals seeking testing for sexually transmitted infections faced a tonne of barriers, including a lack of confidential and convenient testing services and major social stigma that put many off from seeking care. Testing was mainly conducted in specialised clinics or healthcare facilities – and options like home sampling, online access to testing, and rapid point-of-care tests were virtually nonexistent.
Above all this era was characterised by a reactive approach to sexual health, where testing and treatment were mainly sought because of symptoms, rather than as part of routine health care or preventative measures. With as many as 70% of female chlamydia infections causing no visible symptoms and many other infections such as trichomoniasis and gonorrhoea often appearing asymptomatically, it's clear that symptom-based testing has never been enough.
How At-Home STI Testing Changed Everything
The advent of online STI testing has brought about a major shift in how individuals can seek care for STIs. This method lets people get testing kits discreetly, submit samples (such as vaginal samples chlamydia trachomatis), and receive test results via email or text messages.
This approach has significantly increased access to STI testing, especially among young adults, pregnant women, and other groups at increased risk who may face barriers to traditional clinic visits.
The discreet and user-friendly kits can be ordered straight to your home and returned in the mail, with no need to visit a clinic – and the increased access these kits offer has been absolutely transformative in some areas. In fact, one systematic review found that the testing rate using home STI kits was 11 times higher than testing at sexual health clinics in some areas. Particularly for resource-limited settings, for example – like a rural area where the nearest sexual health clinic is a long drive away – at-home testing can make routine testing a whole lot easier.
While people may have been sceptical, at first, about the accuracy of at-home tests, studies show that these can be highly reliable. Results from these kits can be just as accurate as those obtained in clinics, since they use the same labs to analyse samples.
Typically, once received by a lab, sample processing takes an average of just five working days – so you’ll get your results promptly, which can ease the gnawing anxiety of waiting, and speed up the process of getting appropriate treatment where needed.
Improving STI Tests For Better Treatment and Increased Uptake
NAAT
The introduction of nucleic acid amplification tests (NAATs) is a major breakthrough in STI testing, especially when detecting infections like chlamydia and gonorrhoea. These tests work by amplifying the DNA or RNA of the pathogens, making it possible to identify even small quantities of the bacteria with high accuracy.
This technological leap has seriously improved the sensitivity and specificity of STI tests – meaning they’re more reliable at correctly identifying infected individuals and reducing false positives or negatives (because no one wants to be told they’ve got an STI when they…haven’t).
For example, in the case of chlamydia – one of the most common bacterial STIs – NAATs have given us more effective screening in both symptomatic and asymptomatic individuals. Traditionally, testing for chlamydia required invasive procedures (like urethral swabs in men or endocervical swabs in women), which could put people off getting tested. Now that we can use urine samples or self-collected vaginal swabs, the process is way less invasive and more user-friendly. You can easily collect a sample in the privacy of your home, when using at-home testing kits, or in a healthcare setting – without wincing at all those invasive procedures.
Rapid Point of Care Tests
The integration of rapid point-of-care (POC) tests into the realm of sexual health care is another major shift in STI testing, particularly for critical infections such as HIV (Human Immunodeficiency Virus).
These rapid tests are designed to deliver results in a matter of minutes (minutes!), a stark contrast to traditional lab-based tests that could take days or even weeks. We can’t overstate the impact of this massive advancement; especially when considering the importance of early detection and treatment in managing HIV.
Rapid POC tests for HIV typically involve a simple procedure – such as a finger prick to obtain a small blood sample, or an oral swab – with the test processing the sample on-site to give you results almost immediately.
It’s worth noting, though, that if antiretroviral therapy (ART) – which can significantly reduce the virus’ impact on the immune system and decrease the likelihood of transmitting it to others – is needed, healthcare providers would need to conduct a confirmatory blood test prior to beginning treatment. While rapid POC tests are hugely important, ART would not be started based on a POC test alone.
That said – the accessibility and convenience of rapid POC tests have vast implications for public health strategies aimed at combating HIV by making testing more readily available in a variety of settings, not just specialised clinics or hospitals. This means these tests can reach a broader segment of the population; including those who might not seek out traditional testing due to stigma, lack of access to healthcare facilities, or lack of awareness about their risk status. Community-based testing initiatives, outreach programs and even at-home testing kits are now possible, all of which give us a more proactive and inclusive approach to HIV prevention and care.
Tampon Samples
One of the most exciting examples of STI test innovation in recent years is – if we say so ourselves – the development of Daye’s tampon-based sampling process. This uses the simplicity and familiarity of tampons – a menstrual product used by millions – as a way of collecting samples for STI testing.
All you need to do is wear a tampon for a short period of time, then send it back to the lab for testing – a variety of sexually transmitted and bacterial infection types can be detected from this single sample. Neat, right?
The tampon-based approach has been especially transformative in testing for infections like HPV, chlamydia, and gonorrhoea, offering a discreet, non-invasive, and user-friendly alternative to traditional swab or urine-based tests. Particularly for young people or pregnant women who want a more comfortable approach to STI testing – an approach that can be carried out in their own time and in the privacy of their own homes – the tampon sampling method has been extremely successful.
Recognising Mycoplasma Genitalium
Not every innovation in the realm of STI testing is technological; one major innovation in recent years has been the increase in testing for Mycoplasma genitalium. This is known to cause various urogenital infections, including urethritis in men and cervicitis in women, which can lead to more serious reproductive health issues if left untreated, like pelvic inflammatory disease (PID) and infertility.
Testing for this particular STI hasn’t always been simple as all that, though – and often still isn’t.
Testing for M. genitalium has historically been challenging due to the bacterium's slow growth in culture and the need for specialised molecular tests, which weren’t widely available or cost-effective for routine use until recently.
Most importantly, though, Mycoplasma genitalium in itself isn’t tested routinely, because it’s not known if it’s a problem in asymptomatic people; and, crucially, treatments for Mycoplasma genitalium are known to increase microbial resistance. As the BASHH treatment guideline says: ‘The evidence suggests that the majority of people infected with M. genitalium in the genital tract do not develop disease’ – following up with, ‘There is no evidence that screening asymptomatic individuals will be of benefit, and indeed is likely to do harm at a population level’. The CDC, meanwhile, similarly doesn’t recommend screening asymptomatic patients due to the risk of increasing antibiotic resistance by treating patients who, to put it bluntly, don’t need treatment.
Consequently, most services will now test samples of individuals who’ve tested positive for Chlamydia or Gonorrhoea and are symptomatic, as they’re more likely to, subsequently, have a Mycoplasma genitalium infection. You could also get a test if you have a sexual partner who has tested positive for it, or if you are suspected of having pelvic inflammatory disease.
But if you do want to know for sure, some at-home tests – yep, such as Daye's tampon STI kit – can detect Mycoplasma genitalium. This innovation in STI testing means the bacteria can be quickly detected and treated, helping with the management of an infection that could lead to severe reproductive health issues if left untreated.
Combining STI Testing With Other Vaginal Health Tests
We’re all about the innovations today; but yet another key innovation has been the combining of testing for STIs with other types of infections that can impact your vaginal health, like BV and yeast infections.
This holistic approach to vaginal health screening gives you a comprehensive assessment of your health status: multiple conditions can be found (and, if necessary, treated) in a single testing process. You can get a more complete understanding of your vaginal health, leading to targeted treatments that address all conditions, rather than focusing on a single infection. Diagnosis is way more streamlined and treatment is far more effective and efficient, reducing the risk of complications stemming from untreated infections.
For this exact reason, we've created the Daye STI and vaginal health testing kits. These not only look for STIs like chlamydia, gonorrhoea, trichomoniasis, mycoplasma genitalium, mycoplasma hominis, and ureaplasma, but can also identify the pathogens that cause BV and even the presence of candida which causes thrush. Plus, don’t forget our aforementioned tampon sampling process; which is exactly how our At-Home HPV Screen works. All you have to do is insert the Daye Diagnostic Tampon into your vagina, wear it for 20 minutes, remove and post it to our labs; after which we’ll send you a detailed report about your results.
And it doesn't end there; our vaginal microbiome screening can also identify the presence of the friendly good bacteria (lactobacilli) you need to keep your vagina happy. With this more detailed picture of your overall vaginal and sexual health, you can gain a better understanding of everything: From STI acquisition risk factors to fertility implications. If we say so ourselves, it's the holistic approach to sexual health that you deserve.
The Role of E-Technology in Enhancing STI Testing
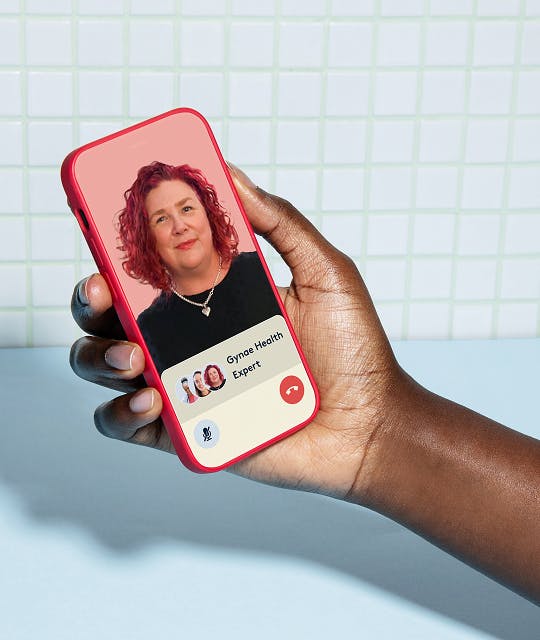
Innovation extends beyond just the types of tests people are using; e-technology has introduced new tools that streamline the testing process, offer rapid results, and facilitate follow-up. For example, Daye’s online sexual health testing platform connects you directly with vetted specialists, helping you access the treatment or personalised health advice you need. (Never let it be said that we don’t prioritise empowering you to take control of your sexual health.) Daye's sexual health online platform allows you to:
- View all your sexual health results and detailed information on a user-friendly dashboard
- Access personalised after-care and treatment options
- Get quick and confidential access to doctors, nurses, gynaecologists, and fertility experts
- Receive lifestyle advice and resources to support your health
Bringing e-technology into sexual health care marks a significant advancement in how people can approach and manage their health. It's a testament to how digital innovation can enhance the accessibility, understanding, and management of sexual health – making it an integral part of overall well-being in the digital age.
The Future of STI Testing: Challenges and Opportunities
Protecting yourself from STIs and safeguarding your sexual and reproductive health has never been easier, thanks to the aforementioned innovations in STI testing over recent decades. However, despite significant progress, challenges remain. Sexual health services are under high demand as STI rates increase, while limited funding for local authorities and clinics also poses a challenge for STI testing.
Nonetheless, the future is hopeful. By embracing new technologies, fostering partnerships between public health entities and prioritising the needs of female and AFAB patients, we can continue to make strides toward a future where sexually transmitted infections no longer pose a significant public health challenge.
The journey is ongoing, but with each new technological development and increased access to services, we move closer to achieving this all-important goal.
Who’s with us?
Related Products
See our Founder’s results!
Wondering what we test for, and what results look like? Enter your email below and Valentina, our Founder, will send you her screening report.
By entering your email above you agree to receive marketing emails and promotions from Daye.