Table of contents
1. Menstrual cycle 101
2. The menstrual cycle and physical health
3. How can I alleviate muscle and joint pain during my menstrual cycle?
4. What are some other coping strategies for physical menstruation symptoms?
Illustrated by Ralitza Nikolova
“I always feel lethargic in the run up to my period,” says Charlotte Millington, 34. “My muscles feel more fatigued and joints like my knees get achey the day before I’m due on.”
Periods – like the absolute treats they are – don’t just impact our bodies by way of menstrual cramps. They can affect our physical health in myriad other ways, like the fatigue and joint or muscle aches that Charlotte mentioned. And these symptoms don’t just rock up during our actual period; they can make themselves known during other parts of the menstrual cycle, too.
45-year-old Daisy White runs and does a lot of bootcamps; and she experiences painful muscles and joints for around 10 days every month, before and during her period. “[The pain starts] about four days before [my period],” she tells me. “It’s like everything creaks and my limbs are really heavy. Specifically, my back and neck always hurt.” Daisy notices that her running times are “very slow during this period”.
For people whose physical health endures days – or even weeks – of pain or discomfort during the menstrual cycle, it can be inconvenient at best, and debilitating at worst.
But before we jump into the science behind how – and why – the menstrual cycle impacts physical health, let’s start off with a brief refresher on the menstrual cycle itself.
Menstrual cycle 101
Monte R. Swarup, MD, FACOG, is a board-certified OB-GYN in Chandler, Arizona; and Founder of the women’s health information sites HPV Hub and Vaginal Health Hub. He outlines the four phases of the menstrual cycle:
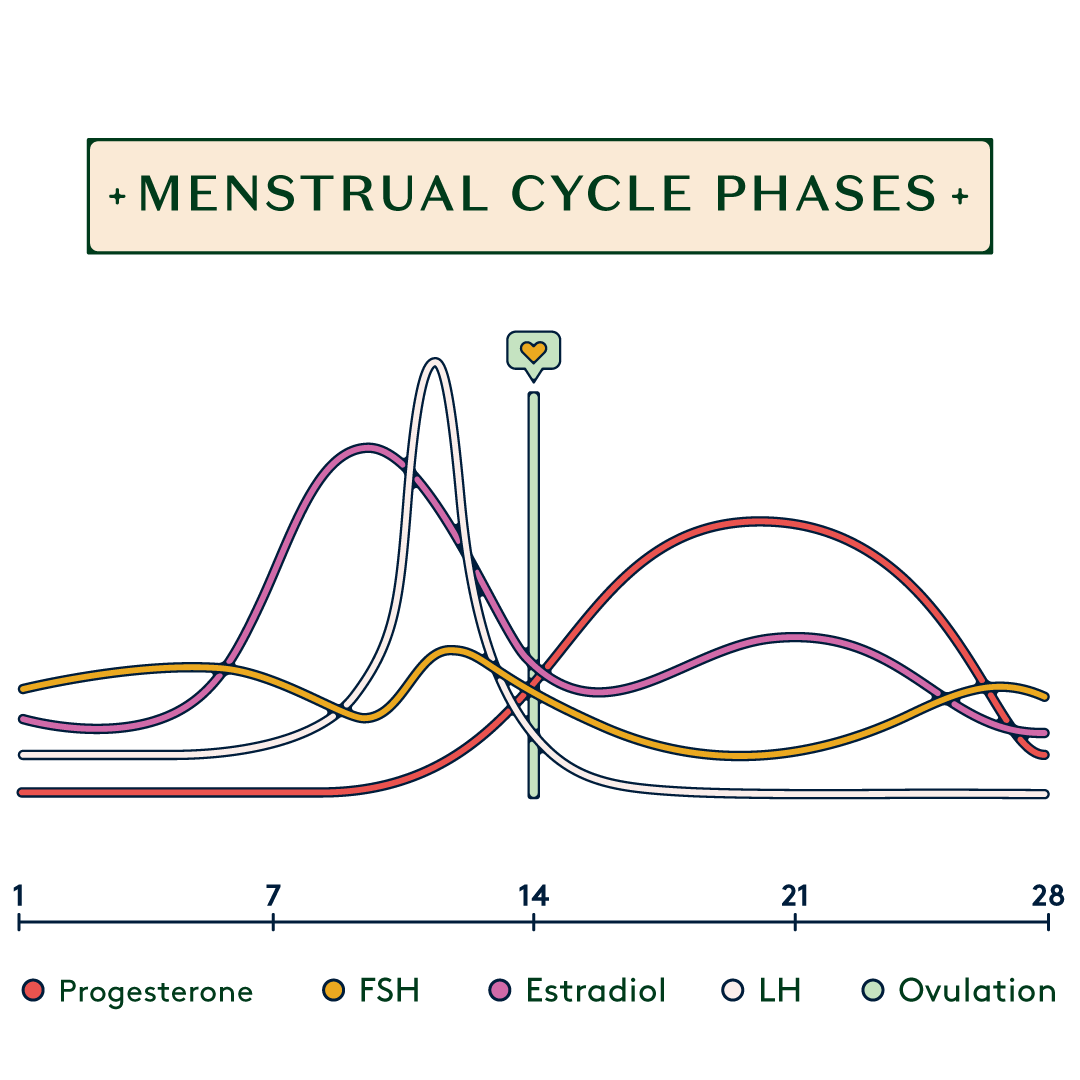
- Menstrual phase (days 1–5): in other words, this is what we know as the period.
- Follicular phase (days 1–13): “This is when egg cells start to grow as the result of being stimulated by hormones in the pituitary gland,” says Swarup. Effectively, sacs known as follicles form in the ovaries and house eggs. One of these eggs will then ‘mature’ – more on this below. Meanwhile, “the inside lining of the uterus develops a lining called the endometrium under the influence of estrogen,” Swarup continues.
- Ovulation phase (day 14): “This is when the ovary releases the mature egg cell,” says Swarup. “The egg cell is swept down the fallopian tube.”
- Luteal phase (days 15-28): “This is when the released egg cell lives for approximately 24 hours. If sperm does not impregnate the egg cell it disintegrates in that time,” Swarup concludes. “Once the follicle releases the egg, the ‘shell’ left behind in the ovary becomes a corpus luteum which secretes progesterone. Progesterone makes the uterine lining ready for a pregnancy to implant. If not pregnant, the corpus luteum dies after 14 days, progesterone goes down and we go back to menstruation.”
So that’s the menstrual cycle, in the briefest of nutshells. Now for why we’re all here; how can the menstrual cycle impact our physical health?
The menstrual cycle and physical health
Well, throughout the follicular phase, you’re likely to be feeling pretty sparkly. “Most menstruating individuals feel very good at this time,” says Melanie K Bone, MD, FACOG, Director of Medical Cannabinoid Therapies at MorseLife Health System and a member of Daye’s advisory board. “They do not experience side effects of too much or too little estrogen or progesterone. For the most part, this is the favourite time of the cycle for many people. The body functions normally and [the] mood is usually stable.”
Then, just before the ovulation phase in the middle of the cycle, things change.
“Signals from the brain and ovaries result in a rapid increase in estrogen levels followed by a surge in luteinizing hormone (LH) about a day before ovulation to trigger the release of the egg,” Bone continues. “The increase in estrogen can impact different people differently. Some feel great. Others complain of[:]
- Headache
- Fluid retention
- Feeling ‘too hormonal’.”
It’s worth noting that, if you’re a budding (or actual) athlete, your physical performance may be on top form during this time. “The LH surge also stimulates a burst of testosterone,” Bone explains. “This can increase libido and overall well being. It would make sense that this phenomenon would increase athletic performance during this time of the cycle."
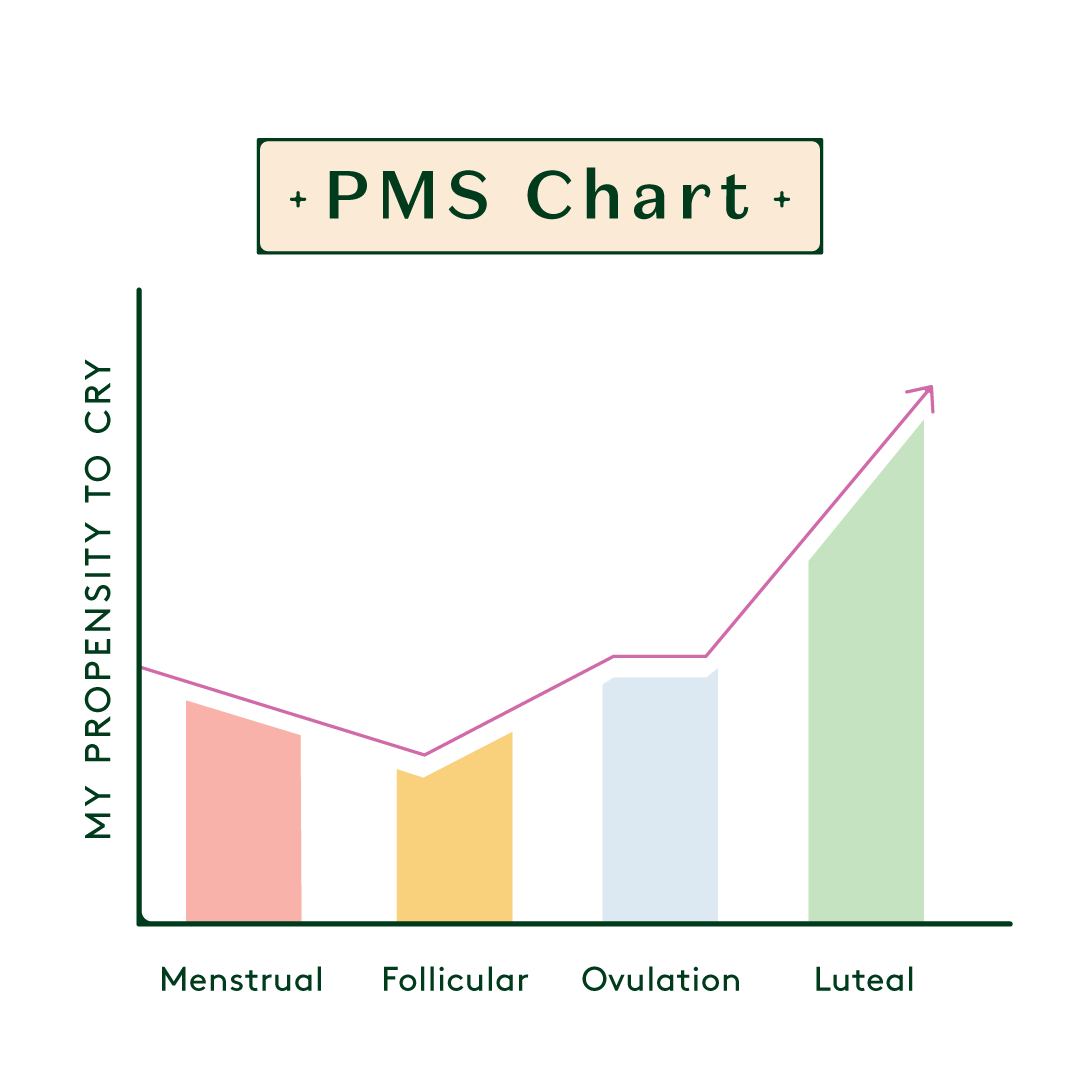
So it’s not all bad, then. But, once we hit the luteal phase, things start changing again. “The estrogen levels start a slow decline until the next period and the progesterone levels start to rise quickly,” says Bone. “This is [...] the time when most menstruating individuals will experience negative phenomena related to hormonal changes” – otherwise known as PMS, or PMDD when very severe.
“While [progesterone] relaxes muscles, which can be beneficial for sleep, it also contributes to bloating and mood changes,” says Bone – in other words, two classic symptoms of PMS. “Joint tightness or stiffness is a side effect of the fluid retention that can accompany the elevated levels of progesterone.”
Bone adds that – more rarely – progesterone can result in “intense breast swelling and tenderness”, together with flu-like symptoms.
And then there are prostaglandins. “It is common for women to complain of aching pain during the luteal phase,” says Bone. “This is less likely about progesterone than the increased secretion of prostaglandins in the pelvis. Prostaglandins are pro-inflammatory elements that generally are well-controlled with non steroidal anti-inflammatory medications [NSAIDs] such as ibuprofen.”
And when the period is a few days away, then – with any luck – the physical symptoms caused by the luteal phase will be out of the way for another month. Then the period arrives, with all its cramps and pain: joy!
How can I alleviate muscle and joint pain during my menstrual cycle?
Firstly, there’s Vitrue Health. Using innovative technology, Vitrue aims to reduce – or entirely eliminate – the impact that those tense, uncomfortable, painful musculoskeletal issues can have. Throughout the process, their go-to approach is a wholly accurate assessment: so they can get to the heart of why your joints or muscles are giving you such grief.
Patients are measured using a single depth sensor (don’t worry; you won’t have anything attached to you!) and the system measures the patient’s performance during a variety of motor function tests. You can also request a specific test; so if your menstrual cycle is repeatedly targeting the same joints or muscles and is interfering with your quality of life, let Vitrue know. Hopefully, you’ll find out what’s causing the pain or discomfort; and then you’ll be able to explore how to actually treat it.
“
“One of the ways we can deal with [it] is by keeping the muscles that stabilise our joints in good condition.”
In the meantime, though, Posture Coach Ana Stefan has some stretching exercises that might help with those joints and muscles:
- “Hip circles and hamstring stretches (with a band) [are] great for reducing the tension and stress from the hips and legs,” she says.
- “Child’s Pose is great for opening the hips and soothing the body,” Ana continues.
- “Cat-cow and cobra stretches [are] fantastic for relieving that period back pain,” she concludes.
Georgia Bondy is a qualified pole fitness instructor and founder of new start-up Well Adapt, which aims to create exercise resources for people with chronic health conditions.
She explains that joint pain and inflammation during menstruation itself is common. “One of the ways we can deal with [it] is by keeping the muscles that stabilise our joints in good condition,” she explains. “That way, when the joints are inflamed, they are under the absolute minimum of pressure. Less pressure can mean less pain. Things like adding a regular hip flexor stretch such as a [Shoulder] Bridge or a reclined hip stretch to your routine can make all the difference.”
Ana adds that her two favourite stretches for menstrual cramps themselves are a supported bridge and a supported heart opener. “These are passive stretches which target the connective tissue,” she explains. “You use props (blocks or pillows, cushions, blankets) and a specific breathing technique to stimulate your parasympathetic nervous system (the rest and digest part of your nervous system) which in turn will allow you to feel more stretched and keep that feeling of being open for longer.”

What are some other coping strategies for physical menstruation symptoms?
“Every individual needs to experiment to determine what works best for their premenstrual complaints,” says Bone. “Combinations of allopathic and complementary approaches usually work best. For example, a good diet with exercise and magnesium supplementation can help alongside taking medications such as anti-inflammatory agents and mood stabilizers.”
And, of course, if you’re experiencing physical symptoms during your actual period (as well as the aforementioned period cramps); there are potential solutions for those, too. “I suffer with bad period pains that cause the muscles in my lower back to tense up,” says Charlotte. “Thankfully, this has been helped recently with some intense physio and the use of a TENS-machine.”
And if you’re looking to alleviate the menstrual cramps themselves, Swarup suggests the following:
- “Take an over-the-counter pain reliever such as ibuprofen”;
- “Reduce stress with yoga or meditation and breathwork”;
- “Apply heat to cramping muscles such as your abdomen and back.”
And, of course, if you’re ever concerned at all – whether that’s fatigue, joint and muscle aches during any part of the menstrual cycle, or bad period cramps – you should always make an appointment with a healthcare professional. Your health is important, and you can never be too careful.






