Illustrated by Erin Rommel
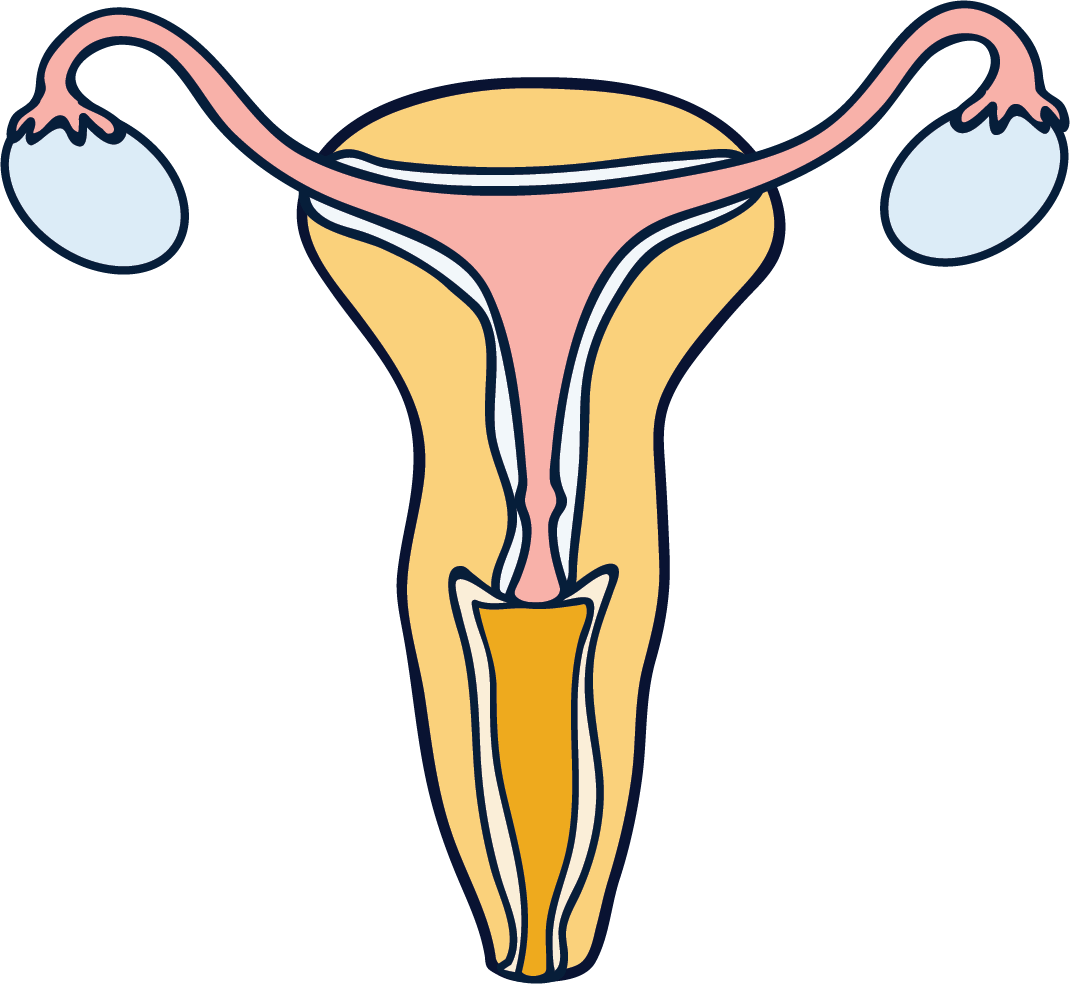
Long COVID – the term used to describe the long-term health effects of contracting COVID-19 – has been linked to damage to multiple organs after the initial infection. Now, there seems to be mounting evidence to suggest that long COVID could affect the reproductive system, too.
Defined as symptoms of COVID-19 lasting longer than 12 weeks (though this timeline can vary), long COVID symptoms include extreme fatigue, brain fog (difficulty with memory or concentration) and severe shortness of breath, among many others.
There have already been concerns about a link between COVID-19 and male fertility, and although we don’t have any conclusive data, recently a connection was made between long COVID and changes to menstruation as well.
An article published in Medical News Today detailed the experiences of six women who reported changes to their menstrual cycles months after contracting COVID-19. Their menstrual changes included abnormally large clots, new cycle irregularity and worsening long COVID symptoms whilst on their periods.
Laura, 24, contracted COVID-19 last March and has now been clinically diagnosed with long COVID by her GP. Her debilitating long COVID symptoms include fatigue, heart palpitations and dizziness, and she is currently unable to work. “Long COVID has had a really drastic impact on my health and quality of life,” she explains.
But the changes to her periods since she contracted the virus have terrified Laura – changes including an alarmingly heavy flow and significantly increased pain. “I had never seen that much blood before,” she tells me. “I didn’t know if the bleeding was even going to stop. It was shocking to me that COVID might’ve impacted my body that much. I frantically Googled to find out how much blood loss was too much blood loss, or how many blood clots were too many blood clots.”
Laura has a strong suspicion that long COVID is behind these changes. “My periods had been consistently light and painless for many years before I got COVID, so the timing of this change has always felt like more than a coincidence to me,” she says.
“I’m already often in pain because of my other long COVID symptoms, so the additional pain I experience because of these new menstrual changes can make life a lot harder. I rely on painkillers to get me through the worst of it, and when that doesn’t help, curling up into a foetal position is sometimes all I can do.”
Laura’s experience is not an isolated incident. Clara*, 47, was taken to A&E with suspected COVID in April, and is now being seen at the UCLH clinic for symptoms of long COVID. She told me of menstrual changes such as clotting, significantly increased pain and an increase in both the flow and duration of her periods. “I would say that my long COVID symptoms [including a burning sensation in the chest and notable brain fog] are worse when I have my period,” she told me. “Also, my PMT is more intense.”
“
My periods had been consistently light and painless before I got COVID
For Michaela, 31, new cycle irregularity has been the main issue. She tested positive for COVID last September: “I was off work for about five weeks, I had a visit to hospital – I had every symptom under the sun,” she tells me.
While Michaela has started to feel considerably better, she is still noticing significant menstrual changes. “Normally, I’m like clockwork,” she tells me, firmly.
“I know what’s coming, and I can plan everything around it. But [in six weeks] I’ve had four periods, and all of them have been seven days. For example, I had a seven day period, then five days off, then I was bleeding again. I’ve never experienced this much irregularity.”
“The healthcare community is in crisis and while healthcare professionals may not have an immediate answer to changes in menstruation patterns, it is not because they don’t care,” says Lynae Brayboy, MD, FACOG, Chief Medical Officer of female health app Clue.
“The reason for this is because there is very limited data. Only one published study from Wuhan, China, has retrospectively studied the effects of COVID-19 on menstruation and sex hormones… the researchers found that on average, sex hormone concentration and ovarian reserve did not change significantly in COVID-19 affected women of childbearing age. It is clear that more research needs to be done.”
Last December, a patient-led research paper examined the experiences of 3,762 individuals who have been ill with COVID-19 for 28 days or more. The paper found that 36.1% of participants with an active menstrual cycle experienced period issues, including abnormally irregular or heavy periods.
The paper also found that more than a third of menstruating participants experienced a relapse in their COVID symptoms either during or before menstruation. This is something that Sophie, 28, can empathise with. After testing positive for COVID back in April, she is now still off work with long COVID. One of her first ever symptoms was an excruciating headache.
“I thought I was having either meningitis or an intracranial bleed – that’s the level of pain I was experiencing,” she explains. “It was like someone was digging all of their fingers into my scalp.”
Although Sophie is still experiencing many persistent COVID symptoms, such as a consistently high temperature, her headaches get noticeably worse when her period is due. “My period’s due this week, and all morning I’ve been on the sofa with an ice pack,” she tells me at the time of interview.
“When I eventually go back to work, my main concern is: is this what it’s going to be like, every month? That I’m going to be catastrophic with my headaches, and can’t come to work?”
Understandably, a considerable concern with regard to the effects of COVID on menstruation is any possible corresponding effects on fertility. “I would encourage everyone who has suffered and recovered from COVID-19 to log all of their symptoms, but especially symptoms of their reproductive health,” says Brayboy.
Catherine*, 32, is currently being treated for long COVID at UCLH, and has been experiencing debilitating symptoms such as severe brain fog and fatigue. After contracting COVID in April, her periods stopped for three months and are now “irregular, light and notably worsen [her] already debilitating long COVID symptoms.”
For Catherine, fertility is a very real worry. “I’m concerned that the menstrual changes might represent fertility issues further down the line,” she explains. “We’d planned on trying for a family this year, although I’m now too sick.”
Of course, the considerable stress of a confirmed COVID-19 diagnosis, or of living with long COVID, may be a factor with regard to disrupted cycles and other menstrual changes. After all, there is a proven link between stress and menstrual disruption. But if one thing’s for sure, it’s that greater research is needed to ascertain whether long COVID might have the potential to affect the reproductive system.
“Scientists and health professionals are missing out on the opportunity to use us,” says Sophie, firmly. “We’re rich data! And – I’m sure I don’t speak on my own here – I would do anything to be regularly monitored, just so [medical professionals] have some sort of awareness, and an understanding of what the hell is going on.” Let’s hope 2021 can bring some much needed answers.
*Names have been changed to protect anonymity