Table of contents
1. When we’re young, we think of menopause symptoms as simply being a bit hot, and a bit tired, and a bit stressed.
2. Lauren, 41, went through early menopause four years ago: and she knows exactly what the cause was.
3. Claire’s journey with HRT has been more complicated.
4. As with so many gynae health conditions, far greater awareness is needed when it comes to the early menopause.
Illustrated by Sabrina Bezerra and Erin Rommel
“I first experienced bleeding mid-cycle when I was 32, in 2008” says Claire, now 45. “This was followed in 2012 by massive loss of confidence; especially with [regard to] driving. By 2015 I had extreme weight gain, periods that were all over the place (46 days, 15 days, 35 days and so on) and fatigue; and I was asking GPs for advice and referrals to gynaecologists and endocrinologists.”
It wasn’t until she was 39 that blood tests revealed what was happening to Claire — at which point her symptoms had expanded to night sweats and mood swings. She was eventually diagnosed with primary ovarian insufficiency (when the ovaries stop producing their usual levels of particular hormones) and early menopause. “I was utterly devastated. Utterly,” she says.
“On one hand, I was delighted that I finally had a diagnosis, and [to know] I wasn’t going mad. I was [also] lucky, because I didn’t want any more children. But going through [early] menopause was devastating to process. It still is. I have to manage this condition every day.”
When we’re young, we think of menopause symptoms as simply being a bit hot, and a bit tired, and a bit stressed.
We might hear the phrase ‘menopausal’ (regrettably and, needless to say, vastly inappropriately) branded as an insult due to the inexplicable stigma attached to the condition (‘She’s so menopausal’, someone might mutter about a middle-aged cis woman); but for the most part, menopause remains a murky, hazy state that we still don’t know anywhere near enough about. And when it comes to early menopause — which can result without warning (and, often, without explanation) — the resulting infertility and health issues it presents can make it a very difficult experience to deal with.
“A woman’s ovaries usually produce an egg each month,” says Menopause Specialist and Clinical Director at My Menopause Centre, Dr Clare Spencer. “But this stops in menopause, which women typically reach between the ages of 45 and 55. Early menopause is when a woman has a menopause under the age of 40. Around 1% of women go through [this], and it’s diagnosed by a combination of blood tests and history. It’s usually made when periods have stopped for about four months, or are very infrequent.”
When it comes to early signs of menopause, these tend to be a variation on what Claire initially went through with her mid-cycle bleeding. “Around 25% of women may have some ovarian function; especially early on, when the ovaries are just beginning too slow down” says Spencer. “This means you might have an ‘out of the blue’ period or premenstrual syndrome: warning signs a period may be coming.” Spencer goes on to outline subsequent menopause symptoms as including “hot flushes, cognitive impairment, difficulties with low mood, depression or anxiety”.
“
"For the majority of women who experience it, there will be no underlying cause"
The causes of early menopause remain a little more difficult — though certainly not impossible — to define. “For the majority of women who experience it, there will be no underlying cause,” Spencer explains. “However, there are a number of known causes. These include surgical removal of ovaries with abnormalities — including cancer, endometriosis or cysts — or removal to help prevent cancer. Other known causes are gene abnormalities (the most common of which are Turner syndrome and fragile X syndrome), autoimmune disease and infections.”
Lauren, 41, went through early menopause four years ago: and she knows exactly what the cause was.
She had her ovaries removed at age 37, due to discovering she is a carrier of the BRCA2 gene which significantly increases her risk of ovarian cancer.
“I knew that, as a result of my ovaries being removed, I would enter immediate menopause,” she tells me. “I thought it would happen the day after the surgery, but it actually took a little longer; it was around a fortnight before I began to notice physical symptoms: [which initially included] hot flushes and night sweats.”
Lauren was prescribed oestrogen-replacement hormone replacement therapy (HRT) around six weeks after her surgery; and she says this was highly effective at managing her menopause symptoms. “However, as time went on I struggled more and more with brain fog,” she tells me. “I forgot things all the time and just didn’t feel like myself; my mood was definitely lower.”
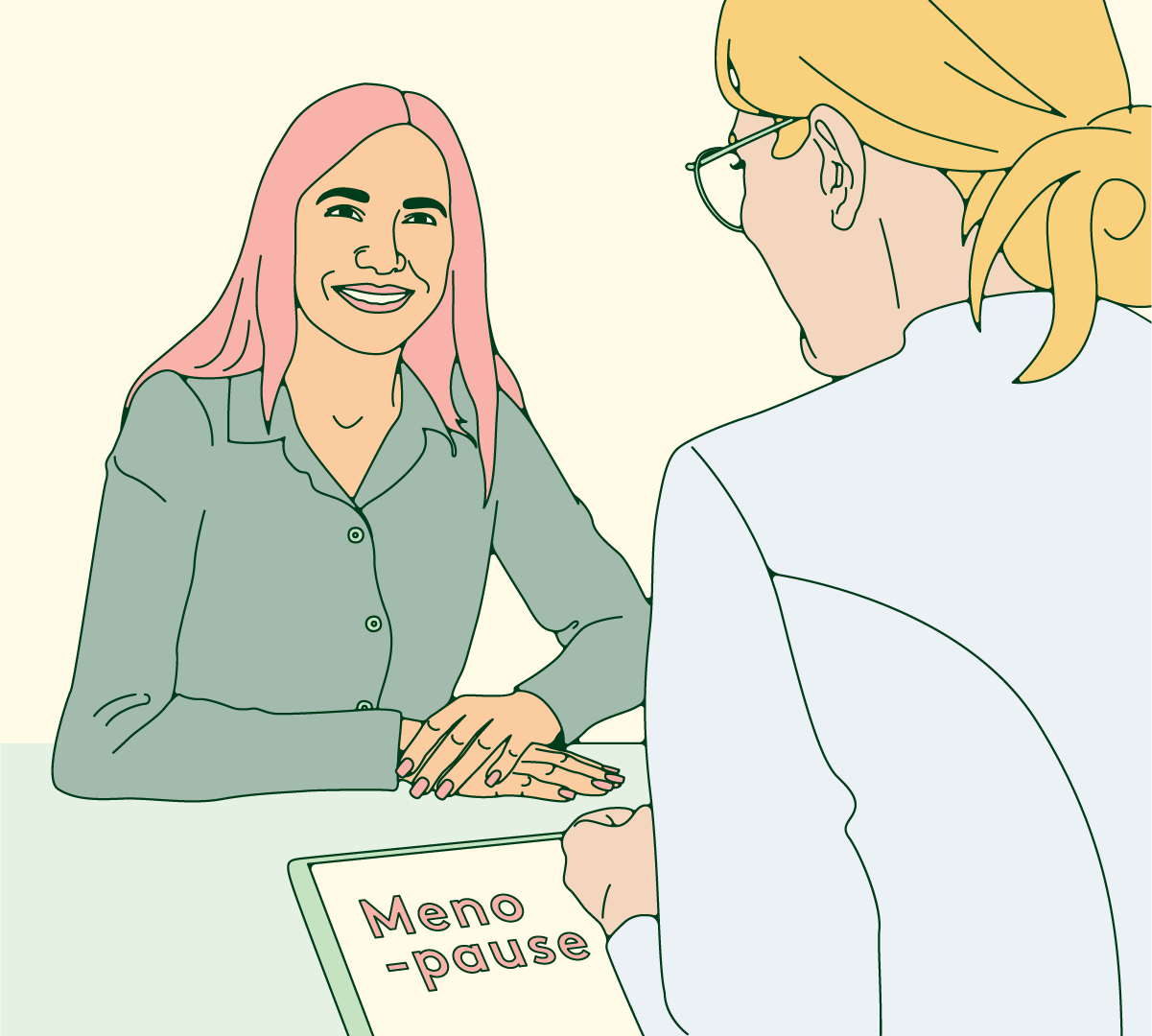
HRT can be a highly effective way to both manage early menopause symptoms and reduce early menopause risks, which a 2015 study listed as including ‘adverse effects on cognition, mood, cardiovascular, bone and sexual health’. The same study concluded that ‘people who undergo premature or early menopause should receive individualised hormone therapy and counselling.’ Spencer confirms that “the good news is that HRT reduces [early menopause risks]”.
Lauren was prescribed increasing doses of oestrogen, but found that this didn’t address her psychological and cognitive symptoms. “It was months later when I was prescribed testosterone,” she tells me. “It was a game changer. I hadn’t realised previously — nor had anyone mentioned — that ovaries actually produce testosterone, and that a decline in testosterone levels can be a big driver in feelings of low mood and cognitive functioning.”
Lauren’s not alone: a study published in 2011 comprising 300 pre- and post-menopausal people found that ‘higher doses of testosterone correlated with greater improvement in symptoms,’ and that ‘continuous testosterone alone…was effective for the relief of hormone deficiency symptoms in both pre- and post-menopausal patients.’
Claire’s journey with HRT has been more complicated.
“The synthetic hormones made me feel horrific; and, while the natural hormones were an improvement, I’m intolerant to some of the ingredients,” she says. “On top of that, I needed testosterone [which I wasn’t offered]. It’s taken six years to get the right hormones, and cost [me] thousands of pounds.”
But now that she’s finally on the HRT that works for her, Claire has noticed a marked improvement in how she feels. “Now that I’ve got my hormones balanced, I feel better than I have since I was a teenager,” she says. “I still struggle with insomnia; but I’m coping and thriving for the first time in a decade.”
Claire doesn’t want to infer that life following the early menopause is easy — “I have to be careful with food, I have to exercise regularly, focus on a positive mindset [and] be vigilant with sleep hygiene” — but she adds that the whole experience has been a blessing, and notes several personal benefits of early menopause.
“
"I’ve had to learn courage; to put my head above the parapet and admit I’m in early menopause, despite the stigma, so I can help others and find deep value in this journey."
Lauren, too, has identified aspects of her early menopause — and the reasons for it — that she’s thankful for. “Of the options I had, the surgery that put me into early menopause is still the right one for me; especially given I have since lost my own mum to pancreatic cancer, which is also on the BRCA2 line. I knew what I was signing up for, when I opted for [the] surgery; but it gives me the best chance of staying around for my son, so it’s been for something — [and knowing] that has certainly made it easier to cope with.”
As with so many gynae health conditions, far greater awareness is needed when it comes to the early menopause.
“It’s essential [that] awareness is raised of the symptoms, and [that] the conversation around [early menopause] is normalised, as menopause is everyone’s business,” maintains Spencer. “Workplaces have a critical role to play in raising awareness, because they can reach so many people; but the education system is also important. Making menopause an essential part of the curriculum will ensure that everyone is aware of the impact an early menopause can have on their health and wellbeing, as well as their fertility.”
We need this awareness; not simply so that we can take early menopause seriously (though we certainly should), but so that the right treatment can be provided as quickly and efficiently as possible. Health risks need to be mitigated, and quality of life needs to be maintained. “A prompt diagnosis of early menopause is important so you can start HRT to treat the symptoms and reduce the risk of long-term health consequences,” Spencer points out. “But doctors don’t always connect the dots, and may not consider early menopause as a diagnosis. If this happens, women can be misdiagnosed as having mental health disorders.”
Misdiagnosis of this sort should not happen; ever. We need to shout about early menopause louder, and discuss the condition without inhibition. We need to know what the early signs of menopause are, and to be able to identify early menopause symptoms. We need to be aware of (and be able to mitigate) early menopause risks, and we should celebrate the benefits of early menopause where they can be found. Nobody should be fearfully confused about what’s happening to their body; and early menopause is no exception.






