Table of contents
1. PMS
2. Painful periods
3. Irregular periods
4. Heavy periods
5. Bleeding between periods
6. Absent periods
7. Conclusion
Medically reviewed by Sarah Montagu (NPs, SRH). Sarah is a highly-qualified sexual and reproductive health nurse with 15+ years of experience.
Illustrated by Sabrina Bezerra, Erin Rommel & Valentin Slavov
If you've ever been concerned that your period is abnormal, you're not alone. In fact, in a survey of girls and young women aged 14-21 years old by Plan International UK, 29 per cent said they have had heavy bleeding, 38 per cent have experienced severe period pain, and 32 per cent have had irregular periods. Yet, more than a quarter also said they hadn't seen a health professional about their worries due to embarrassment.
Every person's menstrual cycle is unique, but it's important to recognise when something might be wrong and take steps to get help. Even though for a long time society has told us to keep quiet about our periods and deal with them alone, there's absolutely no shame in going to a doctor about any of the common period problems listed in this article. While some of these issues might signify an underlying problem that needs treatment, many can be managed with lifestyle changes and medication.
With an estimated 14% to 25% of women and AFAB folks of childbearing age dealing with menstrual irregularities, it's important to understand what is or is not normal for your period. So, let's dive into some of the most common menstrual cycle problems you might encounter. For each, we'll explain how they can be treated and at what point you should think about seeing a doctor for help.
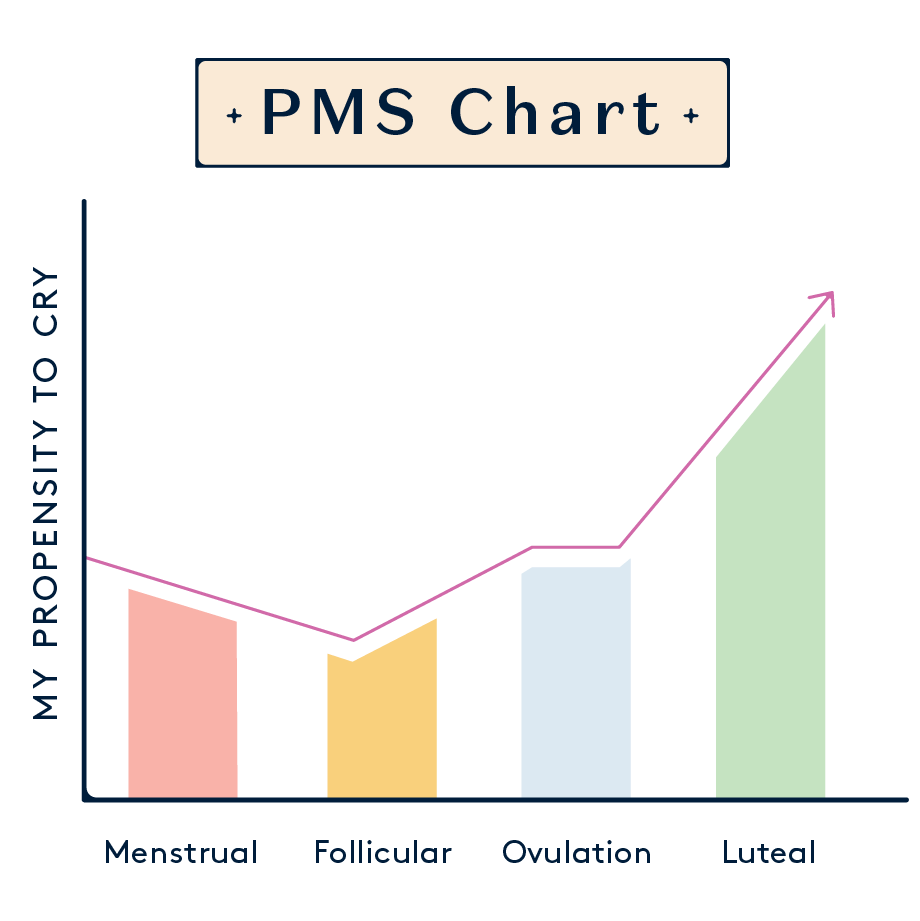
PMS
Premenstrual syndrome (PMS) refers to the symptoms women and AFAB folks may experience in the lead up to their period. While these symptoms may vary between individuals and can even vary from month to month, premenstrual syndrome is extremely common and is experienced by most women at some point in their lives.
Some of the most common symptoms associated with premenstrual syndrome include:
- Mood swings
- Tiredness
- Feeling irritable or anxious
- Bloating
- Breast tenderness
- Stomach pain
- Headaches
- Acne
- Changes to appetite
- Changes to sex drive
Researchers still haven't uncovered the specific causes of PMS, although it's thought that it might be a result of changes in hormone levels at this point in the menstrual cycle.
Solutions for PMS
Usually, premenstrual syndrome can be managed by getting a good amount of sleep, doing regular exercise, eating a healthy diet, and taking over-the-counter painkillers to reduce discomfort. Stress-relieving activities such as yoga, meditation, or a favourite hobby are also recommended to help manage these symptoms.
If these tips don't help, or if you suffer from more severe PMS symptoms (known as premenstrual dysphoric disorder, or PMDD), it's important to talk to a health professional. Your GP can recommend treatment plans such as the combined contraceptive pill to manage hormonal imbalances, antidepressants, dietary supplements, or cognitive behavioural therapy.
To find out more about PMS and PMDD, check out our article about how the menstrual cycle can affect mental health.
Painful periods
Also known as dysmenorrhea, painful periods are very common. However, the level of pain can vary significantly between people, so it may be hard to tell whether your discomfort is part of a normal menstrual cycle or is a sign of something more troubling. While 80% of women experience period pain at some point in their lives, 5-10% of women experience pain so severe that it disrupts their everyday lives.
So, what's considered severe pain? Discomfort for two or three days during menstruation is considered normal, but if that pain continues for longer, or is so severe that your period stops you from going to work, school, or doing other daily activities, that's a sign to seek medical help.
Dysmenorrhea is split into two categories:
- Primary dysmenorrhea: This pain is caused by intense contractions of the uterus during menstruation.
- Secondary dysmenorrhea: This pain is associated with another gynaecological condition such as endometriosis, adenomyosis, pelvic inflammatory disease, or uterine fibroids.
Solutions for painful periods
In addition to taking painkillers such as ibuprofen and paracetamol, lifestyle changes can sometimes ease menstrual pain. These include:
- Quitting cigarettes: Smoking is thought to worsen period pain because it reduces the oxygen supply to the pelvic area.
- Changing your diet: Eating lots of vegetables, choosing foods that are high in fibre, and avoiding red meat and sugary or salty foods can help with painful periods.
- Taking supplements containing gamma linolenic acid (GLA): Evening primrose oil and vitamin B6 are recommended supplements to help fight period pain.
- Reducing alcohol consumption: Alcohol is linked to increased production of prostaglandins, the hormone-like substances which cause contractions of the uterus, and with higher levels of prostaglandins you're more likely to experience severe menstrual pain.
If these methods don't help, it's time to contact your doctor. Prescriptions of stronger painkillers or contraceptive pills can help manage severe pain. Alternatively, non-hormonal medications such as tranexamic acid may be prescribed. Some women and AFAB folks may also opt for an Intrauterine system (IUS)- which is inserted into the uterus, in most people this makes periods lighter or stops them by reducing the lining of the womb from building up. Also used as a contraceptive, this device releases a progestogen hormone which can help reduce severe pain during menstruation.
Irregular periods
While the average length of the menstrual cycle is 28 days, it's not uncommon for the cycle length to vary by a few days shorter or longer than this. However, if the gap between your menstrual periods is less than 21 days or more than 35 days, this is classified as having irregular periods.
Irregular periods aren't necessarily a sign that something is wrong. In fact, many women and AFAB folks find that their menstrual cycle length is very irregular in their teens. In adulthood, irregular periods may be caused by use of hormonal contraceptives, high stress levels, weight changes, exercising too much, or the beginning of menopause.
While irregular periods are not always a major problem, it's a good idea to consult a medical professional about them. If you are trying to conceive, irregular periods can make this more difficult. Moreover, irregular periods combined with other symptoms such as tiredness or weight gain may be a sign of another underlying health condition. For your menstrual cycle and your peace of mind, it's a good idea to get it checked out.
Solutions for irregular periods
Often, there's no need for treatment for irregular periods, unless they are caused by another underlying gynaecological condition. For example, polycystic ovary syndrome (PCOS), endometriosis, or thyroid disorders can all contribute to these irregular period issues, and so the treatment will vary depending on the cause.
The best way to find out the cause of your irregular periods is by seeing your GP to get a referral to a gynaecologist. In addition to a pelvic exam, you may undergo tests such as a pelvic ultrasound to look for uterine fibroids, an endometrial biopsy to test endometrial tissue from your uterus lining, or a hysteroscopy to see inside your uterus.
Depending on the diagnosis, the treatment of irregular periods will vary. Common solutions include hormonal birth control which regulates your menstrual cycle, hormone therapy, or antibiotics if the issue is caused by an infection.
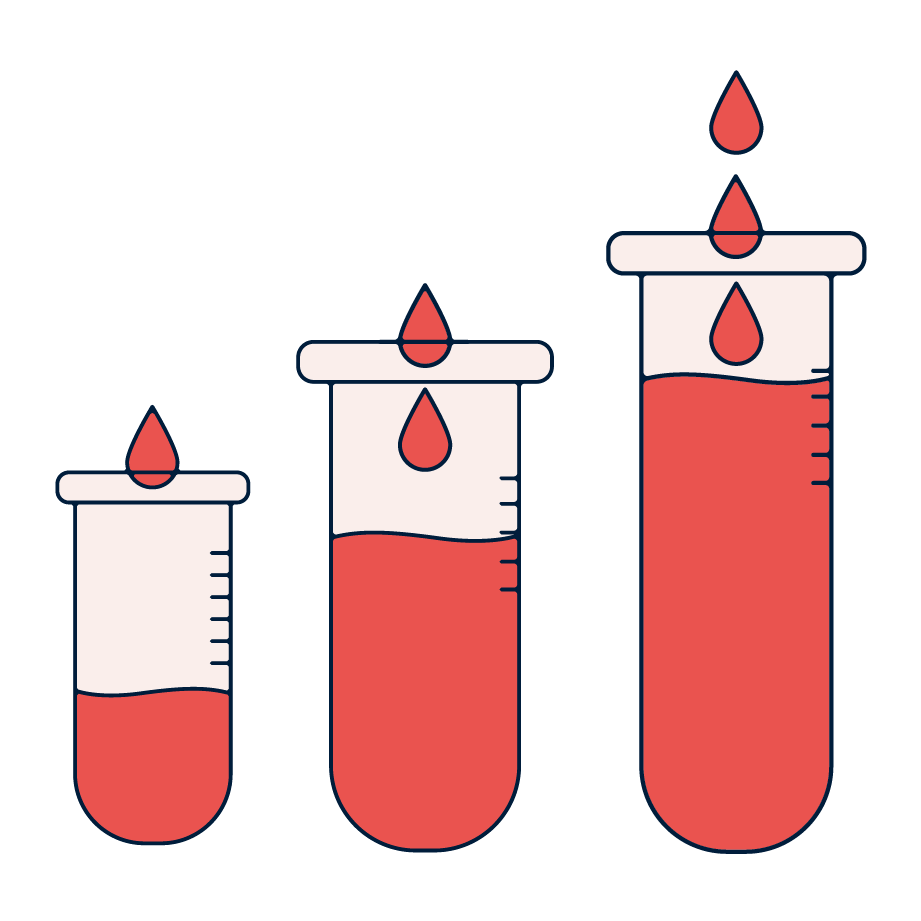
Heavy periods
Sometimes referred to as menorrhagia, heavy periods are defined as excessive bleeding that impacts your quality of life. While impact to quality of life may differ between individuals, some key pointers that you might have heavy menstrual bleeding include:
- Needing to change your tampon or pad every 1-2 hours
- Needing to double up on sanitary products, such as using a tampon and a pad or a menstrual cup and a pad together
- Passing blood clots larger than a 10p coin
- Bleeding through clothing or bedding
- Having to get up in the night to change your period products, or needing to put a towel in your bed when you sleep
- Bleeding for more than seven days
Alongside these signs of heavy menstrual bleeding, symptoms such as tiredness, weakness, dizziness, and shortness of breath may be present. This is because the heavy bleeding can reduce your iron levels and red blood cell count.
Solutions for heavy periods
Contact a health professional if menorrhagia is impacting your daily life. Some solutions to heavy periods include contraception (such as the combined contraceptive pill or an IUS), prescription painkillers, or medication such as tranexamic acid which can reduce the bleeding.
Heavy menstrual bleeding can be triggered by a range of causes, including a recent pregnancy, menopause, or when you first start menstruating. Other conditions that may lead to heavy or irregular bleeding include polycystic ovary syndrome, fibroids, pelvic inflammatory disease, and endometriosis. These underlying conditions can be treated and managed in various ways.

Bleeding between periods
Any bleeding outside of your period is considered abnormal, so it's important to consult your doctor about it. Also known as spotting, intermenstrual bleeding, or metrorrhagia, bleeding between periods is often easily treated but can sometimes be a sign of a hormonal imbalance, infection, bleeding disorder, pregnancy complications, uterine fibroids, or even in rare cases, cancer. While you should always speak to a medical professional if you experience intermenstrual bleeding, it's especially important to seek medical attention if this is paired with fatigue, dizziness, pain, or a fever.
Solutions for bleeding between periods
The treatment for abnormal bleeding between periods varies based on the cause, which can be determined using diagnostic tests such as a pelvic exam, blood tests, a biopsy, or an ultrasound. Depending on the cause of the bleeding between periods, treatments may include contraceptives, medication to address infections, or even surgery to remove uterine polyps.
Absent periods
Technically called amenorrhea, absent periods are not necessarily a problem. Periods can stop naturally during menopause, pregnancy or breastfeeding. In some cases, they can also stop due to intense exercise (in the case of a professional athlete, for example), significant weight loss or gain, or even high levels of stress.
Solutions for absent periods
When looking for solutions to absent periods, it's important to distinguish between two types of amenorrhea. Primary amenorrhea is the term for when a girl doesn't start menstruation by age 16, whereas secondary amenorrhea refers to when previously regular periods stop for more than three months.
Primary amenorrhea can be a result of a variety of different causes, including hormonal imbalances, issues with the reproductive organs, and genetic abnormalities. Depending on the diagnosed cause, treatments may include hormone therapy or treating underlying conditions such as PCOS, eating disorders, or thyroid issues.
Secondary amenorrhea, where a person who previously had periods sees them stop for more than three months, does not always need treatment. For example, it may occur in athletes or in people using particular types of birth control pills or an IUS. As long as it is not causing other health issues or fertility concerns there may be no need for intervention.
However, if the cause of the absent menstruation is an underlying medical condition like thyroid disorder or hormonal imbalance, treatments are available to help regulate periods. For women and AFAB folks who want to get pregnant, fertility treatments can be offered. Weight management and stress management techniques can also sometimes help with the return of regular periods.
Conclusion
Every menstrual cycle is unique, and each person may experience different symptoms and menstrual patterns. However, overly heavy or painful periods, irregular or missed periods, and intense physical and psychological symptoms of PMS all warrant medical attention. For many of these period problems there are quick and easy fixes – there's no need to continue enduring severe pelvic pain or heavy or prolonged bleeding every month!
Here at Daye, we understand the many barriers that stand in the way of getting help with your menstrual cycle. Whether it's embarrassment, lack of access to doctors, or difficulty getting a doctor to believe your symptoms at all, too many women and AFAB folks are struggling to get the medical attention they need.
That's why we created the world-first Period Pain Clinic, a service to help you get answers and personalised treatment plans for your gynae health concerns. By partnering with leading sexual health experts and pelvic pain specialists, the clinic helps you take control of your menstrual health. Plus, it gives you access to innovative treatments and resources to manage your symptoms. For anyone suffering with severe menstrual cramps or who is struggling with the physical and emotional symptoms of their period, it can make a world of difference.






