Illustrated by Erin Rommel
We do a lot of things for our health; we go to therapy, we exercise, we eat nourishing meals, we get regular STI check-ups… so why are so many people with a cervix reluctant to get regular cervical screenings?
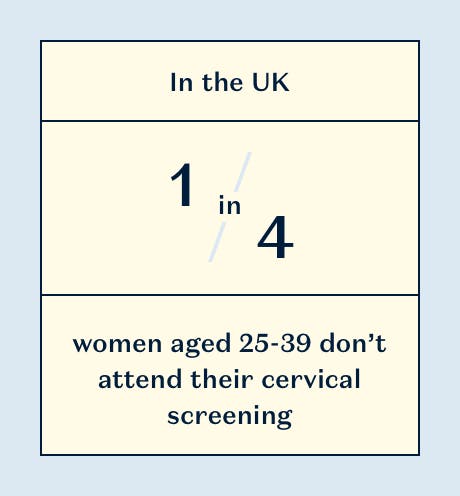
Cervical screening attendance is at a 21-year low, and according to the UK’s only dedicated cervical cancer charity Jo’s Cervical Cancer Trust, 1 in 4 women (aged 25-39) skip their smear test.
In the UK, people with a cervix 25 or over are invited every three years to go in for a smear test. It’s a relatively quick and painless visit, and could potentially save your life. So, why the hesitation?
A survey by Jo's Cervical Cancer Trust found that 81% of women aged 25-35 delay or miss their appointments because they’re embarrassed at the prospect, a statistic that has been at the centre of most cervical screening campaigns. While it speaks volumes that so many women feel uncomfortable getting a gynaecological check-up, for many, the reasons are more serious and complex that just being embarrassed.
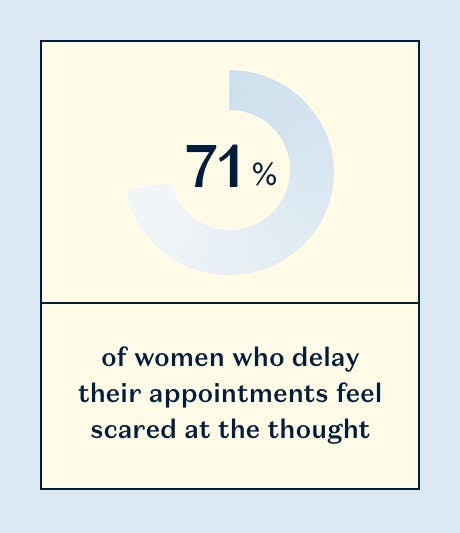
71% of women feel scared and 75% feel vulnerable at the thought of having to get a smear test. While those numbers are disheartening, they’re not surprising.
“There are a wide range of reasons for low attendance,” says Kate Sanger of Jo’s Cervical Cancer Trust. “Some groups can find attending especially difficult, including those with a physical disability or survivors of sexual violence.”
In fact, research from Jo’s Cervical Cancer Trust and Rape Crisis has found that 72% of women who have experienced sexual violence skipped or delayed cervical screening because of their experience. Furthermore, over half said there was no support to help them prepare for the test, and “lack of understanding and sensitivity” among health professionals was a main concern. Considering that 1 in 5 women have experienced some type of sexual assault in their life, that makes for a lot of missed smear tests.
“I think the fact that smear tests are triggering for women who have been sexually assaulted needs to become part of the public narrative around smear tests,” says Lucy, 29, who put off getting a screening for over a year after being sexually assaulted. “For a long time, I couldn’t even stand the thought of a cervical screening—just imagining it would make me become panicky and tight-chested. I think it’s the very literal fact of something alien entering you. I hid the reminder letter for a long time so I wouldn’t have to think about it.”
Lucy chose to get her screening done at a sexual health clinic as opposed to a GP, as she felt they was little support for someone in her situation. “GP surgeries can be quite in and out, you never quite know what the experience will be like. I don’t feel most GPs are adequately trained in dealing with mental health situations, and so I felt reticent to rely on them to understand how triggering it will be. I had to google like mad to find forums discussing it. It seems to me such an obvious trigger.”
Lucy is not alone in her experience, and for people who have suffered trauma or live with chronic pain cervical screenings aren’t as easy and painless as they are for most. “Cervical screening isn’t always easy and that’s really important to remember,” says Sanger. “It can be uncomfortable but shouldn’t hurt. However for others, conditions like vaginismus, endometriosis or feeling unable to relax due to previous bad experiences can mean that screening is not only uncomfortable but can hurt.”
Anna*, 25, suffers from vaginismus and has never had a smear test. “I'm a real advocate for other people getting them—partly why I want to get people talking more about the realities of how scary they can be for some people—but haven't gone myself yet because of my fears around it with my vaginismus,” she says.
“A smear test has been something I've been aware of, and terrified about, since I was about 15. I've never been able to put a tampon in because the vaginismus means my vaginal muscles are like a brick wall. A smear has always seemed pretty impossible and very, very scary. Every time I get a reminder from the GP surgery I feel a sense of panic.”
Even though vaginismus is the second most prevalent female sexual difficulty, Anna says in her experience medical professionals aren’t equipped to offer support because often don't know what vaginismus is, or how it really manifests. “The campaign to get more people to go for smears has been great, but it feels like it hasn't left any room for people who are afraid of going because of reasons other than “I'm a bit embarrassed”. This isn't just a wax we're talking about.”
“The conversation around it really hasn't done anything to allay my fears. It's impressed upon me the critical importance of having my smear test done without actually giving any answers as to how (as in, physically how it will happen if my vaginismus means it's a brick wall situation) or what support I'll be given. Much of the conversation seems to be “yes we know it's awful, like really truly horrible and frankly quite traumatic, but you've got to do it”. That's not helpful, and it doesn't normalise the process.”
“
Every time I get a reminder from the GP surgery I feel a sense of panic.
For people who suffer from endometriosis, the experience is similar. “I never received any support and I always told the doctors and the nurses about my issues,” says Isabelle, 42. “I used to get regular smear tests in my twenties. They used to be uncomfortable, but not painful. However, as my endometriosis got worse, the smear tests would be extremely painful. Just having the speculum inserted would be excruciating. I would always cry during my tests, it was horrible. And after the smear test I would have days of bad period-like cramps that required heavy painkillers. "Take a few Nurofen when you get home" is probably the most "helpful" advice I received.”
“I think the medical establishment needs to acknowledge that for some women cervical screening can be traumatic. It enrages me to no end to see those marketing ads stating how easy it is to have a smear test,” Isabelle says. “They always imply that you're irresponsible or silly to not undergo such a simple test ("maybe just some mild discomfort") that could save your life. For some women it is far more than mild discomfort and it's time we acknowledge that. And maybe research can be done into how to make cervical screening for women with endometriosis or other chronic pain disorders more accessible.”
According to Public Health England, around 2,600 women are diagnosed with cervical cancer in England alone each year, and around 690 women die from the disease (that’s 2 deaths every day). It’s estimated that if everyone attended screening regularly, 83% of cervical cancer cases could be prevented… so for such a life-saving test, there should be more support for people who find cervical screenings painful or triggering.
“Ensuring people know where to access support and information that is written with them in mind is essential. This is equally as true for those that find cervical screening traumatic or painful,” says Sanger. It’s bad enough that millions of women feel embarrassed about getting a necessary gynaecological exam, but by focusing on that as the sole reason so many people don’t get smear tests does a disservice to people dealing with trauma, chronic pain or gender dysphoria (all very valid concerns that should be addressed with care and support).
Everyone should feel comfortable to be in charge of their health, and healthcare professionals play a fundamental role not only in making appointments a safe and supportive space, but also giving women the tools to feel confident in such vulnerable situations. Listening to women and making sure all individuals are accounted for is the only way cervical screening rates will rise, and cervical cancer diagnoses will drop.
If you’re feeling worried or want to talk through any concerns, call the Jo's Cervical Cancer Trust helpline on 0808 802 8000, where their trained volunteers can offer support and tips.
*names have been changed for anonymity.