Table of contents
1. The history of endometriosis diagnosis
2. What are ICD codes and why are they important?
3. What does the future of endometriosis look like?
Illustrated by Sabrina Bezerra, Erin Rommel & Valko Slavov
Endometriosis is a condition that impacts people around the world. In fact, according to the World Health Organisation (WHO), this chronic condition affects roughly 10% (190 million) of reproductive-age people globally, often causing severe pain and discomfort. While there is currently no cure for endometriosis, there is a growing awareness of the disease and an increasing demand for further testing and diagnostic techniques.
One prominent US surgeon, Dr Ted Lee, a Clinical Professor and Director of Minimally Invasive Gynecologic Surgery at the University of Pittsburgh, is leading the way forward with his new research on ICD codes for endometriosis - research he thinks will give patients a more accurate diagnosis and provide healthcare institutes with more detailed data on the condition and how to treat it.
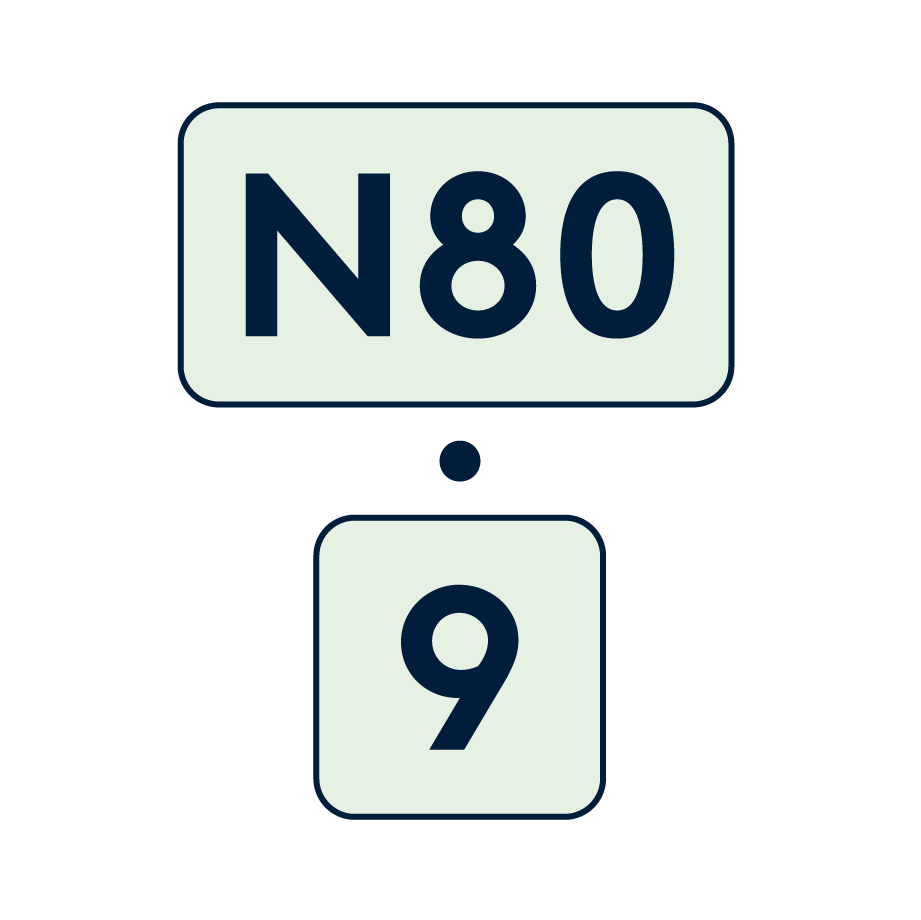
To find out what the future looks like for those suffering from the condition, we spoke to Dr Lee about what spurred him to look into the diagnostic codes (letters and numbers that represent a certain medical condition, procedure, symptom, or disease) for endometriosis. and what the development will mean to current and new endometriosis patients.
The history of endometriosis diagnosis
According to a study by the Journal Frontiers, critical gaps remain in the healthcare system’s understanding of endometriosis and what it means for people. In fact, the study states that if endometriosis was funded by the National Institute of Health at half the level of diabetes, the budget would increase almost 16 times to over $250.4 million annually.
“Sadly, data has shown it takes around eight years for patients to be given a diagnosis of endometriosis,” says Mr Narendra Pisal, a Consultant Gynaecologist at London Gynaecology. “Increasing awareness and specialist access have meant that patients are aware of the symptoms of endometriosis and can confidently approach their doctor to be investigated and seek treatment. However, for a condition which affects nearly 10% of all women, more research is needed for quicker diagnosis and effective non-surgical treatments. It often takes 10 years for any research to translate into clinical practice, so a coherent research strategy is urgently needed.”
Endometriosis affects people of childbearing age, regardless of race and ethnicity, and pain is a common symptom, which is why prompt diagnosis and treatments are crucial.
“The lack of funding for endometriosis research is, in part, why there has been limited progression of endometriosis ICD codes - a system used by physicians to classify and code all diagnoses, symptoms and procedures,” Dr Lee explains. “The reality is that the research into diagnostic codes has been very lacking and this is true in all countries. The original nine codes had been in place since the 1970s and when I began looking into the codes, I was horrified when I realised that a lot of the different endometriosis diagnosis techniques that I was aware of were not codified. There was only one endometriosis code, and that was covering all forms of endometriosis, including endometriosis of the bladder, colon and diaphragm, among other things,” says Dr Lee. “There was essentially no way of diagnosing deep or severe endometriosis when it technically doesn’t even exist,” says Dr Lee. “It took us about three tries over two years, and then the new diagnosis codes finally went live in October.”
For patients, this meant that there was little distinction regarding the type of endometriosis they had, as well as the severity of it. Symptoms of endometriosis can often vary from person to person, but common signs include bloating, pelvic pain, nausea and fatigue. Some people find the condition has a huge impact on their life, affecting everything from relationships to fertility.
What are ICD codes and why are they important?
CD codes are important for distinguishing between different types and variations of diseases and without them, data on conditions such as endometriosis is very limited.
“There are many implications of the new research,” says Dr Lee. “If we don’t have diagnostic codes, how does the government decide that this is an important issue that needs further funding? It’s hard to get the money for research. It’s also validating for the patients to have those specific codes, as they then have a disease that has a code to go with it, rather than just a generic code. “Unfortunately, the new diagnostic codes aren’t going to apply to the UK at the moment,” says Dr Lee. “But, I think what will happen is that now we have this as an example in the US, other countries will hopefully begin to mirror what we’ve done so far.”
For now, the new endometriosis codes are only being circulated in the US, but that’s not to say that this development in diagnostic coding won’t have far-reaching effects.
“New codes define the anatomy as well as the severity of the disease process in much greater detail,” explains Pisal. “This means that different treatment modalities will be coded in greater detail and this will help with assessing the effectiveness of various treatment options for specific case scenarios. With greater access to AI and data analysis, in time we’ll have a greater understanding of the disease process and how to plan an effective, personalised treatment plan. All clinicians will be able to speak the same language using the new codes, which will mean that the research carried out can be analysed in a more meaningful way.”
“
My goal is to start an endometriosis quality collaboration, where surgeons will submit their work and learn from others.
What does the future of endometriosis look like?
“In terms of codes when it comes to endometriosis research, we’re now pretty set,” says Dr Lee. “In terms of endometriosis diagnosis, things are improving and as a result of Covid, the way we can diagnose diseases like endometriosis using is changing. For example, at a conference I was at in Lisbon in October 2022, they were looking at diagnosing endometriosis using saliva that is going to be 97% specific.”
While data and research on endometriosis might be evolving, several barriers, both in the US and worldwide, have made the diagnosis and treatment of the disease difficult.
“When you make a diagnosis accurate and specific, there is a cost,” explains Dr Lee. “Not everyone will have the money to get tested and people with that sort of technology will want to charge. You also have the issue that there are a lot of people on social media who claim to be endometriosis experts, but you don’t know if these people are good surgeons or not and this makes it hard for patients to access proper care. My goal is to start an endometriosis quality collaboration, where surgeons will submit their work and learn from others. The standard of care for endometriosis surgery isn’t always great, so having that peer judgment system will be beneficial for patients. Hopefully, that’s something we can see in the future.”
Efforts to raise awareness of endometriosis have gained huge momentum in the last 10 years and helped to challenge some of the stigma associated with this often misunderstood condition. While the new diagnostic codes are a promising first step in gathering more data, pushing for further research to address the remaining knowledge gaps will help to improve both diagnoses of the condition and treatment of the disease.






