Table of contents
1. How can anorexia impact the body?
2. How can anorexia result in muscle wastage?
3. How can anorexia result in bladder incontinence?
4. Can bladder incontinence as a result of anorexia be resolved?
Illustrated by Erin Rommel, Sabrina Bezerra & Ralitza Nikolova.
“Anorexia nervosa, regardless of body size, can impact multiple systems of the body,” says Jennifer L. Gaudiani MD, CEDS-S, FAED, Founder and Medical Director at the Gaudiani Clinic, which offers expert medical care for eating disorders. “When we consume fewer calories than what our body needs, the body looks to conserve energy by slowing down our heart rate and lowering our blood pressure [...] turning off sex hormones because it’s not a good time for engaging in sex and potentially making a baby, [...] and decreasing feelings of energy so that we can (theoretically) rest.”
We’re learning more about the impacts of eating disorders every day – both physical and psychological – thanks to the efforts of charities like Beat and the courage of people speaking out about their experiences. Take Emma Louise Boynton’s Daye article, for example.
“I felt so alone in the pain and so lost in the thicket of my disordered mind,” she wrote. “There was no escape route from this daily prison in which I’d locked myself. I wished more than anything that someone would just ask me, ‘Are you ok?’ So I could scream at the top of my lungs, ‘NO! I am not OK, I am dying and I don’t know how to make it stop!’”.
But, as with so many illnesses, there’s still so much about anorexia nervosa that we don’t know; and one such little-known result of the eating disorder is bladder incontinence. It’s not unheard of – but it’s also not as widely known as some of the other physical symptoms such as feeling cold or tired, or cessation of periods.
First, though, it’s worth refreshing on the many and varied destructive effects anorexia nervosa can have on the body.
How can anorexia impact the body?
Jessica Kerns MD, FAAP, currently sees patients at Adolescent-Young Adult Medicine in New York City, and previously cared for patients with eating disorders at the Cohen Children’s Medical Center’s Eating Disorder Center at Northwell Health. “Weight loss and malnutrition resulting from anorexia nervosa can affect virtually every organ system, though most of these effects are reversible with improved nutrition and weight restoration,” she explains; and details the physical impacts of the illness as follows:
- “Patients can become very thin in appearance with loss of fat and muscle since the body breaks down these tissues in the setting of malnutrition to produce glucose which is the body’s energy source.”
- “Skin can become dry, acne prone and may develop downy body hair called lanugo.”
- “The cardiovascular system can be affected by slowed heart rate (less than 60 beats per minute), heart rhythm abnormalities, low blood pressure, heart valve dysfunction and fluid in the lining around the heart.”
- Gynecologic effects include suppression of sex hormones including oestrogen, which can result in patients losing their period and other reproductive issues.”
- “Low oestrogen levels can impact other areas of the body including bone, leading to loss of bone density.”
- “Gastrointestinal issues include constipation and delayed gastic emptying.”
And Gaudiani adds: “Anorexia can also cause muscle wasting, including the muscles of the pelvic floor.” Which brings us to bladder incontinence; but more on this below.
How can anorexia result in muscle wastage?
Well, Kerns touched on this above. “In states of starvation, the body generates energy initially by breaking down glycogen, a form of glucose, which is stored in the liver and skeletal muscle,” says Kerns. “Once the glycogen stores have been exhausted, the body breaks down fat tissue into fatty acids and [converts it] into glucose. With prolonged starvation, the liver produces ketone bodies which decreases the body’s glucose requirement.
“Lastly, protein in muscle is broken down into amino acids which are converted to glucose in the liver,” Kerns continues. “This leads to muscle wasting and weakness, and can affect the function of many organs in the body, likely including the pelvic floor muscles which play a role in bladder incontinence.”
“No muscle is immune so this muscle atrophy affects all muscle groups, including the heart and the pelvic floor muscles,” Gaudiani confirms.
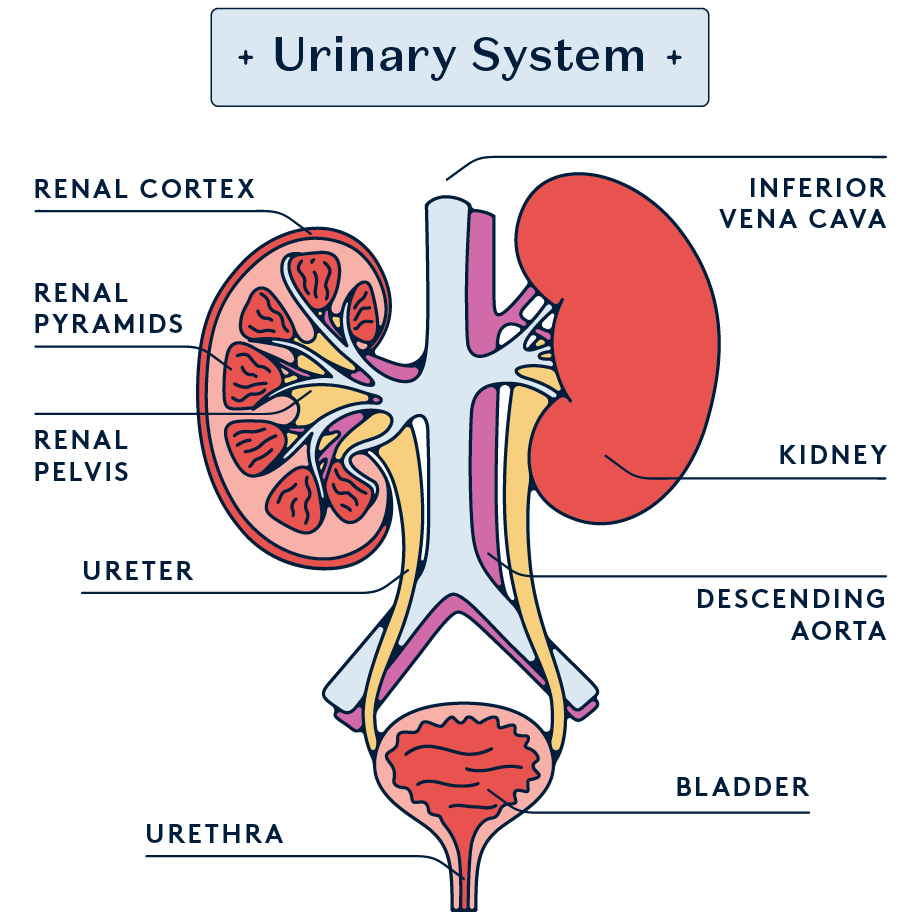
How can anorexia result in bladder incontinence?
First, it’s important to distinguish between different types of incontinence.
- Stress incontinence (SUI): “[This] occurs when there is weakened support of the bladder and urethra, leading to the involuntary leakage of urine during activities that put pressure on the bladder, such as coughing, sneezing or lifting,” says Dr. Melodie Simmons MS, LPC, CEDS-S, ACHE, Founder and CEO of Eating Disorders Revealed in Arizona.
- Urge incontinence: “[This] occurs when there is [...] the sudden and uncontrollable urge to urinate, which can lead to the involuntary leakage of urine,” Simmons continues.
- Overflow incontinence: “[This] occurs with incomplete bladder emptying, resulting in urinary leakage during waking hours as well as while sleeping,” says Kerns.
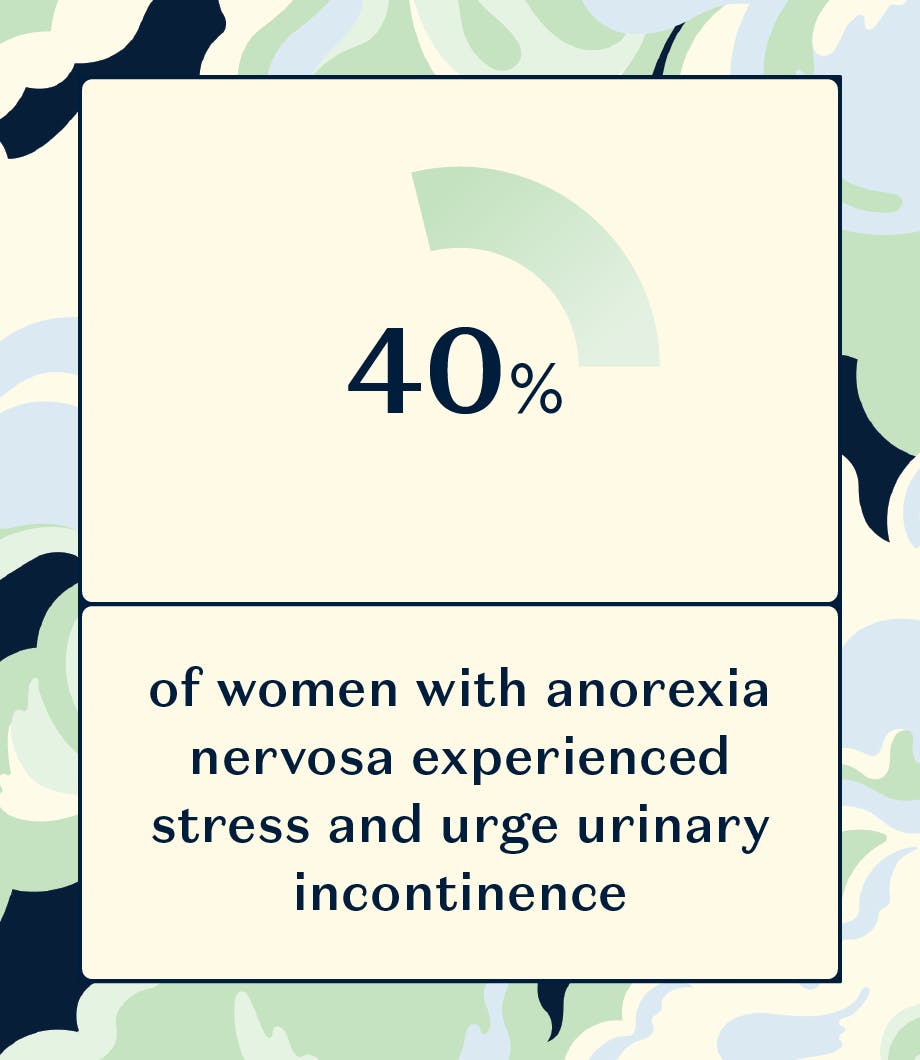
Last year, Femina Physical Therapy quoted research that found ‘40% of women with anorexia nervosa experienced stress and urge urinary incontinence compared with their healthy matched controls’; and a study of children and teens with anorexia nervosa, reported in 2011, found that ‘the overall frequency of daytime and nighttime urinary incontinence symptoms [in participants] was 62.7%’.
So, how exactly can anorexia nervosa result in each of these forms of bladder incontinence?
Firstly, Kerns emphasises that – while disordered eating and malnutrition are associated with an increased risk of urinary incontinence – “the mechanism is poorly understood and is likely due to multiple contributing factors and not solely muscle wasting, though it may be a contributing factor due to its effect on the pelvic floor muscles.”
For example, Gaudiani points out: “If an individual is constipated [...] efforts to push stool out or hold diarrhoea, along with engaging in high impact activities that put pressure on the pelvic floor muscles, such as exercising, also impact the strength of the pelvic floor muscle network.”
But, of course, we can’t rule out pelvic floor muscle wastage as a potential cause of bladder incontinence in individuals with anorexia nervosa.
“Mechanisms for SUI include urethral hypermobility where the urethra, which is the tube that carries urine from the bladder to the outside, and muscles that connect the bladder to the urethra lose the ability to close against the vaginal wall due to insufficient support of pelvic floor muscles and vaginal connective tissue,” Kerns explains.
“Another cause of SUI is poor function of the muscles which keep the urethra closed. Decreased muscle strength and likely resultant weakening of the pelvic floor muscles, low oestrogen levels – which [are seen in malnutrition and] affects urethral blood flow – and excessive exercise may [all] predispose patients with anorexia to SUI,” Kerns continues.
Urge urinary incontinence, too, may have complex causes. “In individuals with anorexia, the cause of urge urinary incontinence may be related to the effects of malnutrition on the bladder muscle or the central nervous system, which regulates bladder function,” says Simmons. “This type of incontinence can result in more significant amounts of urine leakage and may lead to bedwetting, particularly in children and adolescents.”
And overflow urinary incontinence is, again, potentially caused by various factors. “One mechanism is underactivity of the detrusor muscles which control the release of urine from the bladder to the urethra,” says Kerns. “Among many other causes, detrusor underactivity can result from a low oestrogen state. Patients with malnutrition often experience constipation, which is another cause of overflow urinary incontinence due to obstruction of the opening of the bladder by the stool.
So bladder incontinence in patients with anorexia could be due to muscle wastage, yes; but as Kerns emphasised, it’s by no means the only potential cause. In addition to the aforementioned low oestrogen levels, Kerns points out: “A wide variety of medications also increase the risk of urinary incontinence including diuretics, which are sometimes abused in patients with eating disorders. Also, antidepressants and antipsychotics may affect bladder function.”
Simmons adds that psychological factors like stress and anxiety can also play a role here. “People with anorexia nervosa often experience high levels of stress and anxiety, which can contribute to developing bladder incontinence.”
“
Treatment may include pelvic floor exercises, medications or surgery, depending on the severity of the condition.
Can bladder incontinence as a result of anorexia be resolved?
Anorexia nervosa is a highly complex illness and should be treated as such. “It is essential to address bladder incontinence in individuals with anorexia nervosa as part of a comprehensive treatment plan that involves medical management, nutritional counselling and psychological interventions,” explains Simmons. “Treatment may include pelvic floor exercises, medications or surgery, depending on the severity of the condition. With appropriate treatment, many individuals can regain bladder control and improve their quality of life.”
Kerns agrees. “As is the case for most physiologic consequences of malnutrition, nutritional rehabilitation and restoration of body weight can lead to resolution of symptoms, including restoration of muscle mass,” she says. “Pelvic floor muscle training like Kegel exercises can strengthen pelvic floor muscles and reduce incidence of bladder incontinence in patients where pelvic floor weakness is [the] cause of incontinence.”
As with anything, it’s vital to speak to a healthcare professional if you have any concerns. “[It’s] important to note that recovery [...] can take time, and progress may be slow,” says Simmons. “However, with consistent practice of pelvic floor exercises and other recommended interventions, many individuals with bladder incontinence can experience significant improvement in their symptoms over time. It is crucial to work with a healthcare professional, such as a urologist or a pelvic floor physical therapist, to develop an individualised treatment plan that is tailored to one’s needs and goals.”