Table of contents
1. Why are rates of sexually transmitted infections so high?
2. Who is most at risk of STIs?
3. What is the most common STI?
4. What are some STI symptoms?
5. So, how can I get an STI diagnosis?
6. Main STI prevention messages
7. What needs to change in order to help sexual health services cope?
Medically reviewed by Sarah Montagu (NPs, SRH). Sarah is a highly qualified sexual and reproductive health nurse with 15+ years of experience.
Illustrated by Sabrina Bezerra, Erin Rommel & Maria Papazova
'Guessing you've been reading about all these syphilis diagnoses?'
'Can I ask you an awkward question about genital herpes?'
'Am I the only one living in fear of getting an STI diagnosis any minute now?'
These are all questions you might have had good reason to ask recently (yep, even the genital herpes one); because if you've been keeping an eye on the news recently, you may have noticed a particularly worrying story winding its way up the news vine.
Namely, the mounting rise in sexually transmitted infections (STIs) as highlighted by the Local Government Association (LGA).
The LGA represents the councils that provide sexual health clinics – and it’s warning of the astronomical pressure being put on sexual health services in the UK, which are currently buckling under the strain.
In short: STI diagnoses are on the up. According to the BBC, more than two-thirds of council areas have seen sexually transmitted infections climb since 2017. The Guardian added that, during that time, the gonorrhoea diagnosis rate rose in 97% of council areas, while 71% of council areas saw increases in syphilis cases and 36% saw an increase in chlamydia diagnoses.
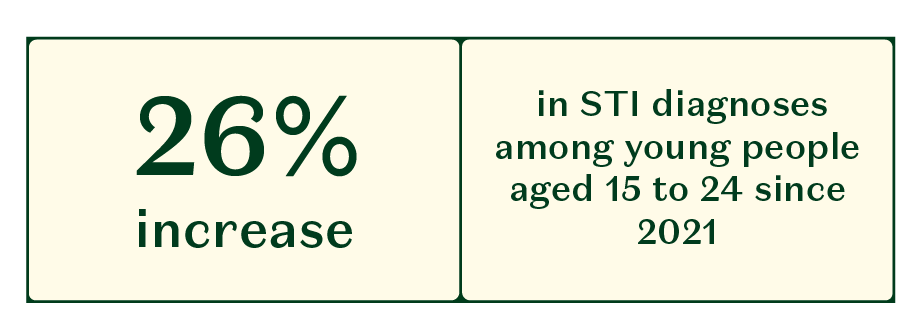
These stats were published in January 2024; but the rise in STIs isn’t unique to this year. Debbie Laycock, Head of Policy and Parliamentary Affairs at Terrence Higgins Trust, says: “The latest UKSHA [UK Health Security Agency] data in England show that STIs are at record highs – more than 1,000 were diagnosed on average every day in 2022 with a 24% rise in rates compared to the previous year. The data shows a jump in the most common STIs, including a 50% rise in gonorrhoea and 15% in syphilis.” Other jumps included a 24% increase in chlamydia and a 26% increase in STI diagnoses among young people aged 15 to 24 since 2021.
Gasping out loud? We don’t blame you. These figures are dumbfounding and terrifying in equal measure; and they get worse. “Rates of syphilis are at their highest since 1948 and gonorrhoea are at their highest since records began,” says Sarah Montagu, Daye’s Sexual and Reproductive Health Nurse.
According to the BBC, gonorrhoea records began in 1918.
1918.
That means gonorrhoea records are at their highest since the year the First World War ended.
Shocked? Us, too – so let’s take a look at just why STI rates are soaring quite so dramatically.
Why are rates of sexually transmitted infections so high?
“Partly, there is an increase in STI testing,” says Helen Burkitt, Senior Sexual Health Nurse at SH:24 and Fettle. “More and more people have easier access to STI testing due to free online services such as SH:24, where you can order a test kit to be delivered discreetly to your home.” Take Daye's STI screen, for example.
As detailed in the Guardian, the LGA said that the rise in STI diagnoses was partly down to increased testing; ‘but also to government cuts to sexual health services’.
And that’s where we really get down to the whys and wherefores. Testing rates are a factor, sure – but, while it's partly behavioural factors explaining the rise in STI diagnoses, testing rates aren't the only reason behind these soaring stats.
Sexual Health Nurse Sarah Montagu pointed to a “reduction in funding to public health and STI services from the UK government”, resulting in “lack of availability of education, testing and treatment”.
She’s right. According to the Guardian: ‘LGA analysis [...] found that the public health grant received by councils had been reduced in real terms by £880m over the past decade, reducing the ability of local authorities to spend on STI testing and treatment’. Now, said David Fothergill – chair of the LGA’s community wellbeing board – ‘local sexual health services are grappling with unprecedented increases in demand’.
“Due to cuts in funding for sexual health services, STI rates might be higher because people can simply not access the services they need, their local clinic may have closed – or reduced its opening hours – so more people are going round with undiagnosed STIs who can’t get the testing and treatment they need,” Burkitt explains.
And Montagu added another reason as to why STI rates might be so high, centred on health inequalities: “High risk groups not being targeted, which increases health inequalities as these groups carry the burden of infection”. Which brings us on to…
Who is most at risk of STIs?
Let’s take another look at the UKSHA data, which highlights the shocking 2022 stats. Speaking on this, Laycock says: “Sexual health in England continues to be a story of inequality with certain groups impacted once again including Black minority ethnic populations, young people, and gay and bisexual men.
“People of Black Caribbean ethnicity had the highest diagnosis rates of chlamydia, gonorrhoea, syphilis, trichomoniasis, and genital herpes,” Laycock continues. “The number of STI diagnoses in gay and bisexual men increased in this period – with rates of gonorrhoea rising by 41% while syphilis saw a 13% rise.”
‘Year after year the same groups are most impacted by STIs, including young people, gay and bisexual men, people living with HIV and those of Black Caribbean ethnicity,’ said Richard Angell, Chief Executive of Terrence Higgins Trust. ‘But nothing is being done to properly understand the impact of structural inequalities on poor sexual health, including racism, sexism, homophobia and transphobia’.
What is the most common STI?
“Chlamydia,” says Montagu. “It is easily passed through unprotected sex; plus, most women or AFAB people (75%) and 50% of men or AMAB people don’t have symptoms.”
We know, of course, from the aforementioned news reports, that gonorrhoea and syphilis diagnoses are soaring, too. Burkitt details some of the other common STIs as including the following:
- HIV
- Genital herpes (HSV)
- Genital warts (HPV)
- Trichomoniasis (also known as TV)
- Mycoplasma genitalium
What are some STI symptoms?
“Often, STIs have no symptoms, so the only way you know if you have one is to test,” says Burkitt. “You cannot tell if someone is more likely to give you an STI; STIs are non-discriminatory. Anyone can have an STI.”
Burkitt details possible STI symptoms for people with vaginas as including:
- Unusual discharge: Green/yellow/frothy/watery/foul smelling
- Pain during or after sex
- Unusual bleeding: So between periods or during/after sex
- Abdominal pain
- Pain passing urine
- Lumps, bumps or sores around the genital/anal area
It’s also worth remembering that STIs are the leading cause of pelvic inflammatory disease (PID), which is an infection that develops in the vagina or cervix and spreads to the fallopian tubes, womb and ovaries. Symptoms include: pain during sex, bleeding after sex or between periods and lower abdominal pain. If you suspect you might have PID you need a face-to-face appointment for diagnosis, it’s vital not to delay diagnosis and treatment – not least because PID increases the risk of ectopic pregnancy, which is when a fertilised egg implants itself outside of the womb, and which is a medical emergency. Symptoms include severe lower abdominal pain on one side, shoulder tip pain and a missed period/positive prenancy test. If you experience these symptoms, seek urgent medical attention.
The following possible STI symptoms for people with penises:
- Unusual discharge: Green/yellow/frothy/watery
- Pain passing urine or an itching/tingling sensation
- Pain/swelling in the testicles
- Lumps, bumps or sores around the genital/anal area
STI diagnoses can be scary; especially new STI diagnoses for those who've never encountered an STI before. But we can't stick our heads in the proverbial sand when it comes to sexual risk – or any health risk, for that matter. Diagnostic tests are vital, and it's crucial that we all know how to access services that can provide these all-important STI tests, as delaying diagnoses and treatment can lead to worse outcomes.
So, how can I get an STI diagnosis?
“By testing!” says Burkitt, simply. “STIs like gonorrhoea and chlamydia can often be symptomless, so you need to test to know if you have one or not.
“If you have any symptoms that suggest you have an STI, you may need to go to your GP or local sexual health clinic for an examination in order for an STI to be diagnosed,” Burkitt continues. “Some tests have to be done in a sexual health clinic; other tests can be done at home" – otherwise known as self sampling kits.
"Self sampling kits mean you do the tests at home (such as vaginal, rectal or throat swabs, urine tests and finger prick blood tests). You then send them back freepost to a lab, where they’re tested and you get sent the results (e.g. by SMS).”
If in doubt, you should always try and access sexual health services; especially if you’ve done an at-home test and the results have come back negative but you’re still experiencing symptoms. “Clinics will usually be able to do a wider range of tests to help find out what the issue is,” Burkitt explains.
Main STI prevention messages
You can engage in STI prevention by practicing safer sex, consistently using condoms and testing for STIs regularly with every new sexual partner and asking partners to screen, too,” says Montagu. “Using PREP if you are in a high risk group for HIV and keeping up to date with vaccinations like HPV [human papillomavirus], Hep B, Monkey Pox and Hep A if you are in a high risk group for those infections.”
Essentially, it's vital to maintain good sexual health by attending sexual health screens, taking STI tests when you can and having open conversations with new or casual partners, in order to avoid an STI going untreated and leading to complications further down the line: Such as pregnancy complications or even cervical cancer.
It also helps to be aware of how STIs can be transmitted from person to person. “Some STIs like gonorrhoea and chlamydia are transmitted by the exchange of bodily fluids as they cannot survive outside the body for very long, so they will be passed either by vaginal secretions or semen, for example,” Burkitt continues. “Other STIs, like herpes and genital warts, can be transmitted via skin-to-skin contact.”
Burkitt also issues a reminder that hormonal contraception, such as the pill, does not – we repeat, does not – protect you from STIs. This is essential to remember if you're sexually active and having condomless sex, especially with casual partners.
But, as we mentioned right at the start of this article, so much of curbing the spread of STIs is outside our control. There’s a certain amount we can do to prioritise good sexual health, but cuts to sexual health services mean these services are overwhelmed, and testing and treatment is being impacted. So, we come to our final question…
What needs to change in order to help sexual health services cope?
“We’re working hard to normalise testing for STIs and HIV against postcode lotteries in online availability but this is being undermined by a system that is over-stretched, under strain and difficult to navigate,” says Laycock. “That’s why we are calling for urgent investment and long over-due change. That includes a commitment to a 48-hour target for access to sexual health appointments, year-round access to free postal STI testing, and for appointments to be booked quickly and easily via an NHS app.” The earlier infections can be caught, the quicker they can be treated.
According to the BBC, the LGA is ‘calling on the government to provide extra funding, as well as to publish a long-term plan to help prevent and treat sexually transmitted infections’. The BBC also quoted Dr Claire Dewsnap, president of the British Association for Sexual Health and HIV, who highlighted ‘the need for a robust national strategy, backed up by adequate funding’.
In short – government action is needed, and it’s needed now. Laycock also identified the need to address structural inequalities and the disproportionate impact of STIs on certain groups: “We have been waiting for years for the Government’s sexual and reproductive health action plan,” she says. “When this action plan is finally launched it must have equity at its heart with targeted interventions for those who need it most.”
Laycock concluded by saying, “Until sexual health is properly resourced, we won’t see the number of STIs heading in the right direction”; and we couldn’t agree more.
A spokesperson for the Department of Health and Social Care was quoted in both the BBC and the Guardian as saying that more than £3.5bn has been allocated to local authorities in England this year ‘to fund public health services, including sexual health services, and this funding will increase in each of the next three years.
‘We continue to work closely with the UK Health Security Agency, local authorities and NHS England to manage pressures on sexual reproductive health services and improve acccess to routine services’, the spokesperson continued in both articles.
In the meantime: Prioritise your sexual health. Keep testing. Know the symptoms, but remember that STIs can be asymptomatic. Make an appointment with a healthcare provider if you notice anything out of the ordinary; and remember, you can call the national sexual health helpline free on 0300 123 7123, Monday to Friday, 9am to 8pm, Saturday and Sunday, 11am to 4pm.