Illustrated by Erin Rommel
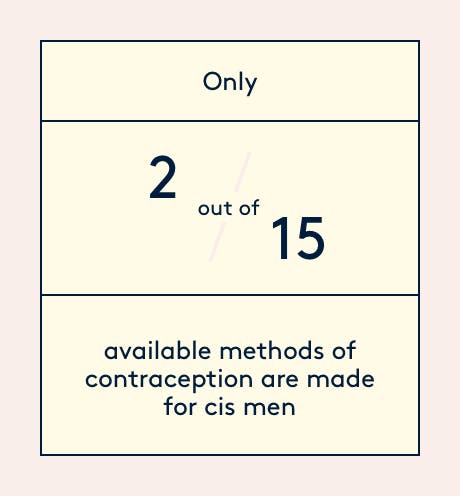
Today, the only contraceptive methods available to people who produce sperm are condoms and vasectomy (male sterilisation).
In fact, the lack of male forms of contraception means women are involved in contraceptive use 90% of the time, even when it involves using condoms—which women often negotiate.
Of the 15 available forms of contraception, 13 are female, and of those only 4 don’t rely on synthetic hormones. Hormonal forms of contraception for women involve manipulating the menstrual cycle with synthetic versions of oestrogen and progesterone, and a large proportion of people using hormonal contraceptives put up with the many negative side effects they can cause—such as acne, headaches, mood swings.
Marco Helliwell, 31, has been with his partner, Anna, for 13 years. She experiences severe mood swings due using hormonal contraceptive methods, and the couple both track her cycle so that they know when to expect fluctuations in her moods.
Her personality changes so much that the couple often spend the days of Anna’s PMS apart, with Marco sometimes booking a lads' weekend out of town, to avoid the nasty clashes that can happen if they’re cooped up in the house together.
“I’ve experienced first-hand how brutal some of the side effects of women’s hormonal contraceptives can be and, to be honest, I’d like to be able to take on some of that burden,” says Marco.
Enter Dr. John Reynolds-Wright, a Community Sexual Clinical Research Fellow at the MRC Centre for Reproductive Health, University of Edinburgh. He is currently heading up a clinical trial, called the ‘Phase 2b Open-label clinical efficacy study’, for a new contraceptive gel for men.
“We’ve been recruiting heterosexual couples to participate and use the gel as their only contraceptive method for a period of one year,” says Dr. Reynolds-Wright.
”We’ve had a substantial amount of interest in Edinburgh and many contacts via telephone and social media, but as the criteria for entry to the trial are quite strict, only a proportion of those interested are eligible to participate.”
Men apply the gel to their upper arms and shoulders every day and then attend clinics to monitor their sperm count. The gels contains the hormones testosterone and segesterone acetate (a synthetic form of progesterone), which causes testicles stop producing sperm.
The research team at the University of Edinburgh hope that couples in long-term relationships could eventually use the gel as an alternative to the female contraceptive pill.
Dr. Reynolds-Wright explains that for many years there has been a lack of interest from the pharmaceutical industry in developing a male contraceptive method.
“For many public bodies the priority has been to develop effective female contraceptive methods—quite rightly it can be argued, as women face the burden of unplanned pregnancy. But also, male contraceptives are technically more difficult to produce. Female hormonal methods (mostly) prevent ovulation which occurs once a month, whereas a male method has to prevent sperm production which happens millions of times each day.”
So, there’s no denying that male contraceptives have got “more work” to do in terms of stopping pregnancy. Development of male hormonal contraception has been happening to some extent since the ‘70s, but in the last decade there have been several high-profile clinical trials focused on contraception for men—in the forms of pills, injections and gels.
Unfortunately, though, many have been blighted by high self-reported rates of side effects such as changes in mood, libido, depression, headaches and acne. Many pundits argue that these are all reactions that women often put up with while taking hormonal contraception.
However, Dr. Reynolds-Wright clarifies that trails can be cut short due to the frequency of side effects, rather than the severity.
The severity of side effects reported by men are often taken more seriously than those reported by women, but we can change this bias by everyone talking about their issue more openly.
Luckily, public perception seems to be shifting as well. In a 2005 study of over 9000 men aged 18-50, 28.5-71.4% of those surveyed expressed willingness to use hormonal contraception.
Earlier this year, Dr. Christina Wang, Co-principal investigator and lead researcher at LA Biomedical Research Institute and her team made significant progress in bringing the male pill to the market. However, Dr. Wang says that there is a lot to do before the pill would be close to being distributed, as researchers will next need to conduct similar studies but on a longer-term scale, using thousands of couples who would be willing to test the drug for a number of years.
Dr. Reynolds-Wright urges people to approach pharmaceutical companies directly to ask them to invest and partner with public institutions to develop male contraceptives further and bring them to market soon—and to register for a clinical trial, as birth control should be the responsibility of both parties.