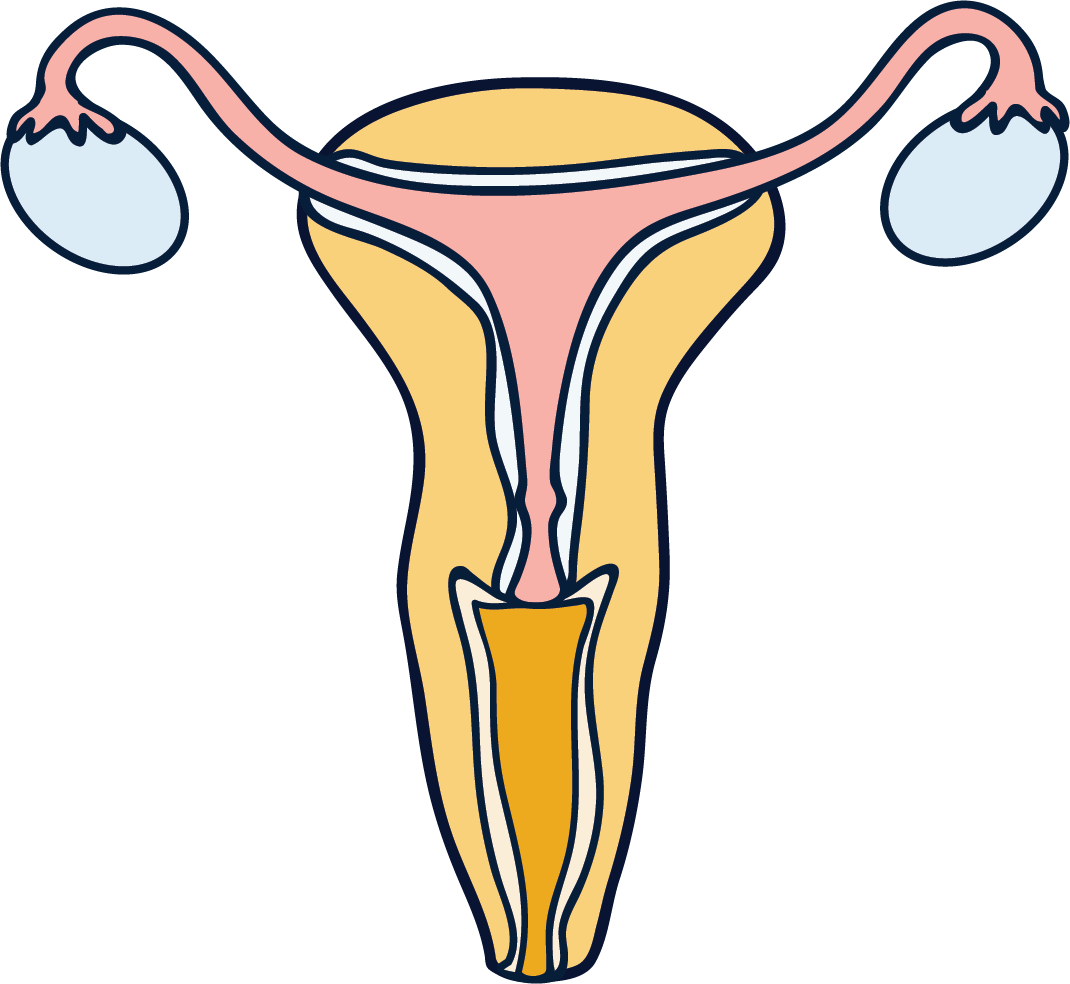
Adenomyosis is a condition where the inner lining of your uterus (the endometrium) grows into the muscle layer of the uterus (the myometrium).
Adenomyosis is often compared to endometriosis, and in many ways they share similarities as they’re both disorders of the endometrial tissue that lines the inside of your uterus. However, they affect the uterus in slightly different ways.
While endometriosis is tissue similar to the endometrium that develops outside the uterus (and sometimes also on the ovaries and fallopian tubes), in adenomyosis the tissue that should be lining the inside of your uterus instead grows within the muscle wall.
Much like with endometriosis, the endometrial tissue in adenomyosis responds to the hormonal fluctuations of the menstrual cycle, thickening and then breaking down. As the old endometrial tissue has no way of leaving the myometrium, it can cause inflammation and pain.
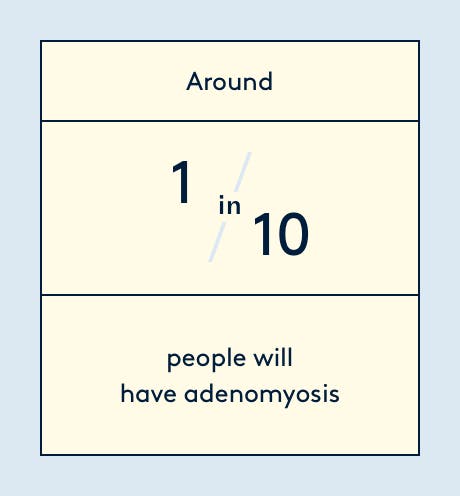
Diagnosing adenomyosis isn’t a straightforward process (another unlucky trait it shares with endo) so it’s unclear how many people it affects, but it’s estimated that around 1 in ten women will have adenomyosis.
Adenomyosis can occur in any person who has periods, but it’s most common found in women aged 40-50 (it only affects around 20% of women below that age), and in women who have had children.
We want every body in the Universe to have the most unproblematic period possible. This is why we designed the world's first tampon for when your uterus is throwing a tantrum. Give feel good periods a try with our clinically validated CBD period care range.
Adenomyosis symptoms
Adenomyosis is a benign condition, but although it's not life-threatening it can cause painful and debilitating symptoms.
Adenomyosis is thought to be asymptomatic in one in three people who have it, but when symptoms do arise, they most commonly include painful and heavy periods. Other common symptoms of adenomyosis are:
- irregular bleeding
- pre-menstrual pelvic pain
- painful intercourse
- painful urination and bowel movements
Because the condition causes very heavy periods, people with adenomyosis have a higher risk of iron deficiency (anemia), which can cause fatigue and dizziness.
It’s also been speculated that adenomyosis might affect fertility. Although there aren’t any studies to confirm that adenomyosis reduces your likelihood of conceiving, the condition has been found in women who have trouble getting pregnant. The main theory is that adenomyosis affects how the endometrium functions, potentially impairing implantation.
What causes adenomyosis?
No one really knows why adenomyosis happens – so you can add that to the quasi-infinite list of female health conditions that remain misunderstood.
Researchers seem to believe that adenomyosis is a hormone-dependent dysfunction. It typically disappears after menopause, when oestrogen levels decline, but it’s likely that your genetics and immune system play a role as well.
Adenomyosis also often goes hand in hand with other gynaecological conditions, like endometriosis (20% of the time) and uterine fibroids (50% of the time), making them potential risk factors.
Adenomyosis is also more common in women who have given birth via Caesarean sections, or have had other uterine operations. The theory behind this is that something goes awry during the healing process and causes endometrial tissue to grow within the myometrium.
Diagnosis
Adenomyosis is often misdiagnosed, mainly because its symptoms (painful periods, irregular bleeding, pelvic pain, etc) vary from person to person, and are shared with many other conditions.
Adenomyosis can be mistaken for endometriosis, IBS, pelvic inflammatory disease or perimenopause.
On top of that, there isn’t a consensus on what the diagnostic criteria should be, so it can take years to receive a correct diagnosis for adenomyosis.
Almost half the time, adenomyosis can be diagnosed through a transvaginal ultrasound. If that fails, you may need a magnetic resonance imaging (MRI) scan.
How to treat adenomyosis
The challenge in correctly diagnosing adenomyosis (and knowing what causes it) means there is no straightforward treatment to the condition. Most available treatments address individual symptoms, rather than the root cause of the condition.
Treatments for the pain and heavy bleeding caused by adenomyosis involve over-the-counter painkillers, or hormonal treatments like the mini pill and IUS. They keep the uterine lining thin throughout the month, reducing or completely preventing your endometrium from shedding when you have your period.
In some cases, doctors may recommend a non-surgical procedure called uterine artery embolisation (UAE), which cut off blood supply to the unwelcome endometrium, causing it to shrink. However, UAE isn’t a permanent solution and it’s not recommended for those who want to conceive in the future.
The last case resort for adenomyosis is a hysterectomy, which involves surgically removing the uterus (and therefore potentially getting rid of the issue once and for all).
TL;DR
- Adenomyosis is a condition where the endometrium grows into the muscle layer of the uterus.
- Around one in ten people have adenomyosis and it’s most common in women over 40.
- It’s often mistaken for endometriosis, a very similar condition.
- Adenomyosis can cause painful, heavy periods, irregular bleeding, pelvic pain, painful intercourse and bowel movements. Around one in three people won’t have any symptoms at all.
- The cause of adenomyosis remains a mystery, which makes diagnosis difficult.
- Treatments for adenomyosis range from over-the-counter painkillers to surgeries like hysterectomy.