To my knowledge, I don’t suffer from endometriosis (she says, touching wood manically) – and thank God, because I know how debilitating it can be.
You’re reading Vitals, so you likely already have knowledge of and interest in reproductive health conditions affecting those assigned female at birth. You’re probably also aware of the by-now-infamous statistic: That endometriosis affects around 1 in 10 people with wombs.
But just in case you need a refresher, endometriosis is the name given to the condition where cells similar to the ones in the lining of the womb (uterus) are found elsewhere in the body.
Symptoms of endometriosis can include extremely painful (or heavy) periods – an idea that makes me viscerally shudder, given that I experience enough toe-curling, fist-clenching menstrual cramps each month and I don’t even have endometriosis –, pain during or after sex, or pain when peeing or opening the bowels. To say endometriosis can interfere with daily life is a vast understatement, especially during periods; plus, there’s the mental toll, too.
And then, of course, there's endometriosis and fertility.
Does endometriosis impact fertility?
Here at Daye, we hate scaremongering; so let’s start by hammering home the following point: If you have endometriosis, that does not – repeat, does not – automatically mean you’re infertile.
What it does mean, though, is that you may encounter more difficulties conceiving – and, further down the line, with pregnancy – than those who don’t have the condition.
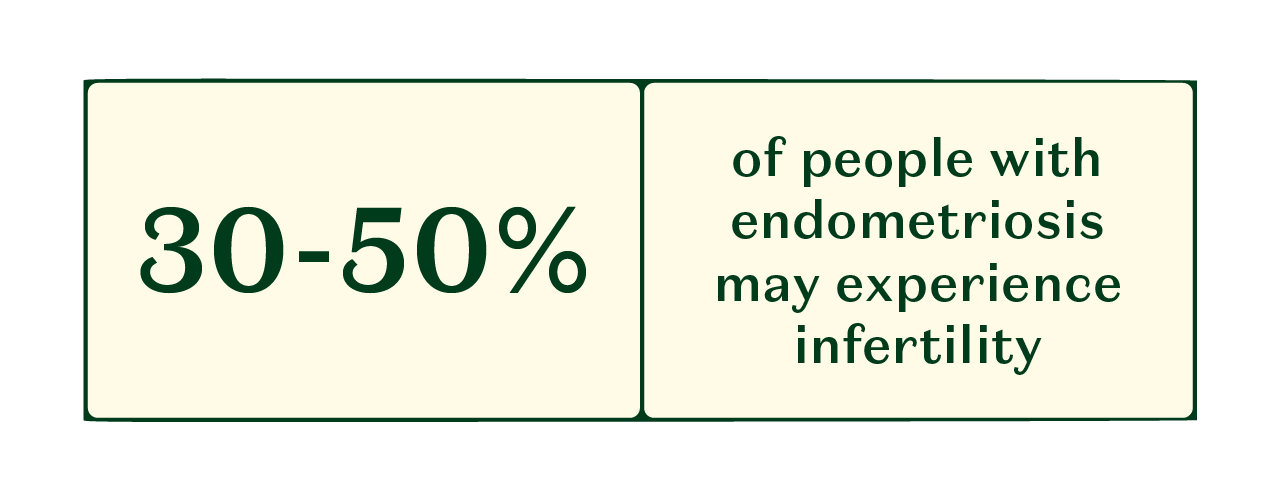
The Fertility Center at Massachusetts General Hospital points out that 30-50% of people with endometriosis may experience infertility. They dive deeper by explaining that people without endometriosis have an approximate 10-20% chance of getting pregnant, while the chance for people with surgically documented cases of endometriosis is 1-10%.
“Endometriosis can cause inflammation [and] create scar tissue, which can affect the ovaries and fallopian tubes,” says Amit Shah, Consultant in Reproductive Medicine atFertility Plus. “This can hinder the movement of the egg and sperm.” AsHealthline put it, ‘If [someone] has endometriosis in [the] fallopian tube lining, the tissue may keep the egg from travelling to the uterus’.
Can endometriosis affect egg quality?
“Deeply infiltrating endometriosis, which grows under the peritoneum, and ovarian endometriosis (endometriomas) are more likely to be associated with infertility,” says Shah. “The severity and location of [the condition] can also influence fertility.”
Christiansen adds that, while “severe or advanced endometriosis is more likely to lead to complications with fertility and pregnancy, it won’t necessarily cause ‘infertility’,” adding: “There are options for women with endometriosis who wish to conceive.”
So, without further ado, let's jump into how endometriosis might affect fertility.
What are the odds of getting pregnant with endometriosis?
Let’s start with some stats. “Whilst endometriosis is associated with fertility problems, natural conception is still possible, even for women with severe endometriosis,” says Christiansen. “It’s estimated that 60-70% of women with endometriosis can get pregnant naturally.”
If you read those odds and feel a quiet swell of hope inside you – that’s wonderful. Because, as the above stats indicate, there certainly is hope that endometriosis-sufferers can get pregnant naturally.
But we’d be remiss if we neglected the remaining 30-40% who might struggle trying to get pregnant; and who might (justifiably) be wondering: How do you ‘fix’ endometriosis for fertility? What should a person with endometriosis do if they're struggling to get pregnant?
“For those who are struggling to conceive naturally, options include undergoing surgery to remove patches of endometriosis tissue, or trying a fertility treatment such as IVF [in vitro fertilization] or ICI [intracervical insemination],” Christiansen continues. “Your doctor will be able to advise on the best next steps.”
And if you’re wondering which fertility odds apply to you, your best shout is to consult a healthcare professional. As Shah says, “The odds of getting pregnant with endometriosis vary depending on the severity of the condition, age, and other individual factors.” Everyone’s journey to getting pregnant will be unique, and should be treated as such.
How does endometriosis affect pregnancy?
It’s a valid question. Let’s say you suffer from endometriosis and have managed to get pregnant – it’s a joyful moment, certainly, but it’s totally fair to worry that you may not be out of the woods yet; to wonder, in short: Can you have a successful pregnancy with endometriosis?
“Some studies show that women with endometriosis can be at a higher risk of experiencing complications during pregnancy, such as preterm birth, miscarriage or caesarean delivery,” acknowledges Christiansen.
Tommy’s is a charity that researches the causes of pregnancy complications, together with how to prevent them, and points out that ‘some medical research has found that having endometriosis increases the risk of placenta previa [...] when the placenta attaches lower down in the womb and covers the cervix’. In this instance, you might be recommended to give birth earlier than your due date or have a caesarean section. The charity also suggests that endometriosis might increase the risk of an ectopic pregnancy, possibly because ‘endometriosis scarring may interfere with the ability of a fertilised egg to reach the uterus’; but adds that more research is needed to confirm this.
But it’s vital not to panic, or to assume that you automatically have an increased risk of these issues if you're pregnant and have endometriosis. “Not all women with endometriosis will experience complications during pregnancy,” Christiansen explains; adding that doctors should monitor your pregnancy closely to keep both you and your baby safe.
Shah agrees. “While endometriosis is associated with a higher risk of complications in some cases, such as preterm birth or caesarean section, it does not necessarily increase the risk of miscarriages or placenta previa,” he says. “Each individual’s experience can vary, and women with endometriosis are often able to have successful pregnancies.”
How can I be fertile with endometriosis?
“If you have endometriosis or suspect you might, [...] then visit your GP if trying for a baby,” Christiansen advises. “NICE (National Institute for Health and Care Excellence) guidelines state that if there is a known predisposing factor for infertility, then doctors should make an earlier referral for specialist consultation. A specialist can take you through options to optimise your fertility.” Christiansen adds that, in moderate to severe cases, treatment options may include those listed above.
Shah adds that, “Lifestyle changes and managing symptoms can also be helpful” and Healthline indicates that some of these lifestyle changes can be done with the aim of reducing inflammation in the body, such as ‘eating nutrient-dense foods rich in fruit, vegetables, whole grains and lean proteins’. In other words, endometriosis, your diet and getting pregnant could be linked.
Some parting tips…
“Some fertility drugs can cause endometriosis to flare so it’s important to get additional support from your treating specialist when going through any hormone stimulation for fertility treatment, should you need pain medication,” Christiansen concludes.
And Shah offers some final thoughts. “It's important to understand that endometriosis is a complex and chronic condition,” he says. “Early diagnosis and a multidisciplinary approach to treatment can improve fertility outcomes. Research is ongoing, and new treatments and understandings of the disease are emerging. It's crucial for women with endometriosis to have access to specialised care and support.
“Remember, individual cases vary, so it's essential to consult with a healthcare provider for personal medical advice,” he concludes. Amen to that.


.png?ixlib=gatsbyFP&auto=compress%2Cformat&fit=max&w=1080&h=1080)